“Radiation.” ☢️
Across the globe, it raises up negative connotations. No one sees a radiation warning image and is “calmed”. Consider nuclear reactors, where radiation is used for a non-carbon energy format, even there we don’t like to use it due to fear. Within medicine, I think everyone’s first thought is: radiation is bad. The rule after all is “As Low As Reasonably Achievable”. Recall the uproar in the population as we added low dose imaging to airport screening. So it is any real surprise that we face an uphill battle as we attempt to convince others of the tremendous value we create? I don’t think so. And now, we have “data”.
The study for today is out of Europe looking at articles within the NY Times and it demonstrates just how pronounced this bias has become.
The rise of negative portrayals of radiation oncology: A textual analysis of media news
It’s an interesting article that backs up what many have stated in the past. We fight an uphill battle. First, some of the details on the approach of the paper. I think these help emphasize that, in fact, this was a real effort to see if there is a slant to the literature - it is far more than just opinion.
It started with every NY Times article ever in print - back to 1851 and then narrowed the field down to 646 articles which, according to the article, were individually read and reviewed by two people. The end result was a selection of 342 articles. And from that we got this data.
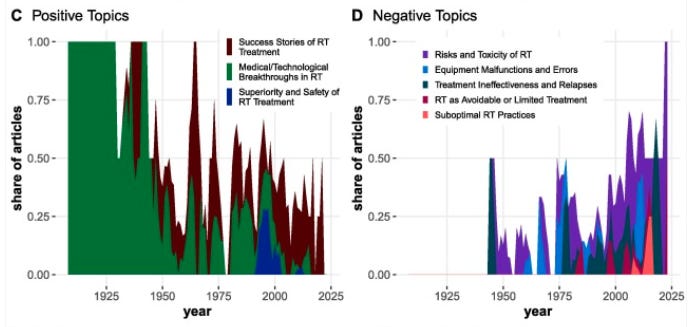
In the image on the left, the number of articles seemed to have peaked about 10 years ago and on the right image, you can see a decline in positive articles and an increase in negative articles.
Below we see a bit more breakdown of the trend for both positively and negatively slanted articles - the declining positive topics on the left and the increasing negative topics on the right.
Note that medical / technological breakthroughs in radiation have been completely replaced with risks and toxicity of radiation.
Where the article missteps is not performing the same type of analysis on medical oncology articles - i.e. showing that today we aren’t just more skeptical of everything - some days, it sure feels like it. But I’ll come back to this with one recent example where I think you can see the answer…
Regardless, whether you look to the New England Journal of Medicine or the NY Times, we aren’t grabbing headlines.

Add to this the massive imbalance that we see in dollars between the pharmaceutical industry and radiation and we have a huge uphill battle. I discussed this difference in a dedicated piece here that focuses on the scale of this financial imbalance:
That piece, written the week of the LIV Tour / PGA merger, starts with this statement, which in light of today’s topic and the recent going’s on at OpenAI, I think remains on point:
If you believe that billions of dollars do not impact outcomes - Ask the PGA tour. Ask our US government who, as the economy turned south looked to Saudi Arabia amongst others to increase oil production. Idealistic positions in the face of massive dollars too often today do not hold up under the weight of these imbalances.
Which brings me back to a major focus of this Substack:
Radiation in Oncology represents a huge value.
Compared to pharma approaches, we take care of more people at a lower cost. Period. Not even close.
Here is a illustration of that difference comparing Radiation Oncology to the Top 2 Cancer Drugs:
4.2 billion dollars for 340,000 patients vs. 5.5 billion dollars for 88,000.
1.22 billion per 100,000 patients vs. 6.25 billion per 100,000 patients.
Per patient, we are over 5x as cost effective in our treatments as two of the leading drugs - with a larger percentage of patients receiving curative / definitive treatment resulting in a much higher value radiation approach.
Now consider just a few of the home runs that I have discussed in the past few months alone - from SBRT for prostate cancer, liver, renal, and lung. To the large impact we are seeing in metastatic settings from a variety of trials. It has been a great year of progress, yet let’s look at a current example and see how we are represented today in the media all to often.
This is the example that the paper uses and I’ll repeat it as it is the best example of the bias. The PROSPECT trial LITERALLY showed that up front chemotherapy given more intensely for a longer period of time to “avoid radiation toxicity” increased Grade 4 toxicity by ~4 times.
(Grade 3 is generally a hospital event, Grade 5 is death, Grade 4 is therefore really bad) (Ref - toxicity data is buried in the appendix - hidden far from the headlines. Prior to surgery, Gr4 Adverse events: 52 of 580 in the chemotherapy arm and 13 of 508 in the chemoradiation arm).
Even patient reported acute toxicity was worse with chemotherapy in 12 of the 14 acute metrics (radiation worse in 1, and one is a toss up). And finally, the trend for overall survival if anything (very slightly) favors combination treatment with chemotherapy and radiation (LINK to X post).
Yet, despite the data, the NY Times headline ran with:
I want to be clear. After backlash and pushback, the “brutal” was removed. But just consider that article in contrast to the study findings. And I’m not arguing radiation is clearly better here - here I think the discussion is nuanced. What is NOT nuanced is that headline. Remember, in the broader context of rectal cancer, we are moving towards 5 radiation treatments (down from 25 for many of these cases) and using a combination of chemotherapy and radiation to avoid surgery in some cases - especially for those patients that might require an ostomy. It is currently one of the most debated and most varied areas of first line cancer therapy. And frankly, it is that broader context, beyond the trial, that amplifies the gross ignorance of the title.
Too often today, we see narrative over data in the “news”, nearly always aligning with dollars.
And then back to Keytruda - a drug that is about the size of all of radiation oncology while treating far fewer patients - Merck spends approximately 2.2 billion on advertising budgets. And amazingly, the media then shows support for drugs (sarcasm). Medical Oncologists, the physicians that give the chemotherapy in the PROSPECT trial, prescribe this drug and many others which fund / advertise the media and so their answer fits well with the business model of media companies. I don’t think it is any more complex than that.
Back in February, I wrote this piece after the results of a radiation trial showed that radiation avoidance was an option for some women with early breast cancer.
The scientific article ran in the NEJM and did show no difference in survival, but it did show local recurrence of the cancer increase from 1% to 10% (I’m rounding (0.9% to 9.5%) if you didn’t have radiation. If a drug did that, how would it be marketed? It reduced the chance of breast cancer recurrence by 10 fold. Mammograms don’t have near that effect size on outcomes. Are there places where I have recommended patients avoid radiation for more than a decade - yes. Again nuance vs. headlines.
These are important societal issues as we attempt to create “value” within our healthcare system.
A prevailing narrative of this Substack is to emphasize the value and strength of radiation oncology as a specialty. In places, I believe we’ve been our worst enemy. I’ve argued this in a handful of articles - too many to include - but we need to shift our language. We must appreciate that it is us against the world at times. We are a small market team being outspent on the playing field by magnitudes of dollars. To compete, we must be more focused and outperform.
We played a part in this
I actually put more of the responsibility within our own house than from those outside the walls of our small community. Beyond the walls they are often just mirroring a lot of what we are saying / doing in our own work.
And I want to spend just a moment and discuss what I think I’ve seen in my 25 years of clinical practice. I think there are some important events that have happened over those decades and it is important to note that there is a collection of pressures that are unique within the US and unique in important markets beyond the US that are pushing us in one unified direction.
US Market:
I’ll go quickly, but IMRT payment rates started imbalances within our market. Government set them, but we ran with them. That money and the push for proton centers with large scale outside investment each created wedges in our market.
On the IMRT side, we pushed back against UroRad models - the urologist jumping into the radiation business and siphoning off all the prostates. We pushed back at first with targeted approaches but then with larger anti-kickback and Stark law arguments. Later this shifted to a broader “Choose Wisely” which I’ve summarized before as “treat less often, treat with less fractions and when you can, please don’t treat”.
Did we compete and attempt to right-size IMRT payments? In my market we didn’t. We tried to lean into “rules” to limit the competition. About 15-20 years ago, I was booed out of the C-suite when I even suggested cutting our IMRT rates to dis-incentivize the urology group from making the large initial capital investment.
And protons were the other wedge. Massive outside dollars rolled into centers that, well before proving clear benefit, relied upon the treatment of prostate cancer as its main focus on every early proforma for the large early passive scanning multi-room facilities. It was followed by aggressive marketing campaigns that far too often grossly overstate benefits and this combination created a toxic environment that did the opposite of unifying our specialty.
And so beyond the walls of our small field, people heard the bad things. The overpayment and abuse. The self-proclaimed over treatment and massive spending alongside other experts rightfully pointing out a lack of data.
And that was in the US…
Beyond the US:
Beyond the US, where we have a glutton of investment and technology, many countries struggle to have enough equipment. In most regions, there aren’t enough machines to treat those that need radiation. The pressures there are quite different from the US market, but ultimately they push us in a similar direction - at least from beyond the walls.
In the UK for example there are tens of thousands of patients waiting months for treatment. Canada struggles with access as well and if you listen to those from India, one of their major concerns is maximizing machine throughput to match growing number of patients that need treatment.
And so the scientific answer is to eliminate or reduce radiation indications or hypofractionate. That is what the physicians must do in those environments. And that is what they have worked hard to demonstrate: that less can be as good - or better - or close enough (depending on the exact situation). It is the only lever that physicians can pull when large bureaucracies hold the purse strings and decide how and where capital resources are allocated.
And ultimately pressures on both sides of the pond push us towards a similar result. But beyond the wall, you loose this perspective and I can imagine that they sound quite similar. The differences fade but the broad impression remains unified » a shift towards less. And the perspective beyond the wall has been affected. And they “align” with the dollars in the pharma / rad onc playing field. And it aligns with everything that human civilizations have known about radiation. And that creates quite an opportunity for clicks via a simple narrative - drugs good, radiation bad.
Just to be clear, right-sizing the treatment is critical. It is good science. It is good for our patients and it increases our value. I’m just pointing out the broader context that several external forces support the narrative.
I see the glass half-full:
Fortunately, I see the tide shifting. I think we are beginning to appreciate the value we bring to the table and fortunately, the math and dollars back us up. I believe there are good signs that we are moving towards a period of greater unity. I think we are demonstrating massive progress for oncology patients and unifying around the understanding that we’ll be a short, efficient, super-high value addition for many oncology patients. We are moving quickly, in many treatment indications, towards a non-invasive alternative to surgery. And so I think the messaging beyond the wall will shift - if we are diligent and persistent.
We can overcome this.
An Analogy: Do you fly?
People fly and when they do, they often get x-rayed to board the plane and when they are up in the air, with less atmosphere, they get more radiation. People move to Colorado, yet the background radiation there is about 5x my home state of Arkansas - every 2 years that difference is about as much radiation as full body CT. 50 years in the mountains - 25 full body CT scans (Ref). 50 years in the mountains - about 10,000,000 airport screening (200,000 x pelvis only CT x 50 - Ref). But yet, I still hop on a plane and fly to the high country. I love to ski and love the mountains.
I don’t like extra radiation - don’t make that mistake - heck, I’m at a proton center because I believe we can do better, but our field is a great asset in the fight against cancer and life systems are amazingly complex. End of the day, we provide tremendous value and even small shifts in our priorities and in our words can be impactful to the long-term success and trajectory of our field.
If Radiation were a drug?
If radiation was a drug in the PROSPECT trial let’s just consider an alternate headline.
New drug (radiation) allows for a large scale reduction in chemotherapy doses. At the same time, it reduces severe toxicities to about 1/4th of our prior approach. And in other studies, this new drug appears to allow us to safely avoid surgery for some rectal cancer patients - especially important for those traditionally requiring a permanent ostomy. Amazingly, that same drug earlier this year demonstrated a 10 fold reduction in breast cancer recurrence if given after surgery.
Yep, pretty sure it would have been written up differently.
But remember, it isn’t just the journalists - we push our value far less than other specialties, thinking somehow it “raises” our integrity. I saw this on X and it fits in well. Consider the difference in how Medical Oncologists will present findings vs. the more “measured” Radiation Oncologist.
Anti-PDL1 treatment is active on surrogate endpoint (pCR) in curable MSI rectal cancer patients based on 12 patients, follow-up of 9 months -> urgent approval and prompt integration into guidelines is required.
SBRT doubles PFS in oligometastatic esophageal cancer patients with limited salvage options in phase II trial -> "more data are needed"
So remember our words matter and how we represent our small field eventually diffuses into the media and population. Don’t just use this study to blame others. At the same time we push the outside narrative to change, we must also look in the mirror and see if we can likewise, do better. We fight a wall of dollars that often seeks to drown out our value - after all, if we are gone the “addressable drug market” increases.
To me, this article drives home the importance of the need to - as I’ve described previously - have the pendulum swing back towards the middle. Focus on outcomes and prioritize optimizing our benefit within the oncology space and focusing on the value we create. The rest will follow. Kudos the authors on taking an idea or “feeling” and turning it into some level of data.
If you made it this far, consider hitting the like button. It helps and guaranteed, takes less time than what it took me to put this together.
Next week we return to data - a new study released with bittersweet timing.







Can you do the math based on a more recent quarterly earnings report from Merck?
"Merck's popular antibody treatment Keytruda, which is used to treat several types of cancer, booked $6.34 billion in revenue, up 17% from the year-earlier quarter."CNBC