SBRT: Renal Cell Cancer. 100% control rate
Not an exaggeration - a zero local failure prospective trial. FASTRACK II
Perhaps grant me just a touch of liberty, but in San Diego over a glass of wine from somewhere in South America, Dr. Siva recalled his first look at the FASTRACK II trial data. From my memory, it was something like this (read with Australian accent for best effect):
I get the data and look at the results. We had no failures. Not one. So I pick up the phone and start calling everyone. Not to celebrate but rather to ask “Just check and re-verify your data.”
2023 - What a year with another big win for patients treated with radiation!!
Radiation continues to repeatedly demonstrate outstanding results. Another great study - this one was released about a month ago in San Diego at ASTRO. I’ve been busy so it took me a second to get to it, but add it to your studies to know and add renal cell cancer to a list of indications where radiation can expand our footprint and deliver value to more patients.
The FASTRACK II trial looked at patients with unresectable or high surgical risk renal cell cancers and gave 1 or 3 fractions of high dose radiation. At nearly 4 years of follow-up. 100% were controlled locally and not a single person passed away from their disease. From a patient perspective, one or three completely NON-INVASIVE procedures, similar to getting a CT scan - cured the disease 92% of the time at 5 years.
Today, we’ll go a bit deeper and look at the data that was presented and ramifications from that trial as we care for patients. We’ll discuss how it impacts options and how we are expanding into areas that historically we didn’t treat.
FASTRACK II trial
(Focal Ablative Stereotactic Radiotherapy for Cancers of the Kidney) TROG 15.03 (Original study design document)
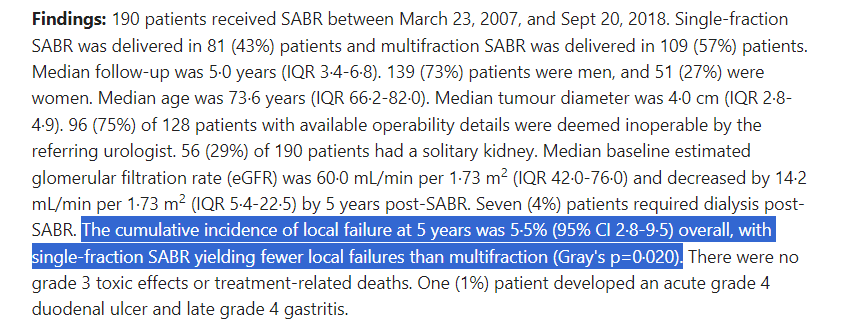
If there is a criticism, it is that this is a small study - 70 patients. Target population were those that were medically inoperable or high-risk for surgery.
Additional patient criteria:
Biopsy confirmed - single lesion
eGFR>30mls/min
Tumor not abutting bowel
10cm or less
Radiation Planning Details:
26 Gy x single fraction - 4cm or less
42 Gy in 3 fractions - tumors larger than 4cm
ITV»PTV - 5mm expansion
99% of PTV covered by 100%
Max dose - between 125% and 143%
Below is the OAR table from previously published design document - pertinent for any clinical implementation.
Tumor characteristics:
Importantly, just note, these are not small tumors. Average lesion size was 4.6cm ranging from 1.5cm to 8.9cm
FASTRACK II Results:
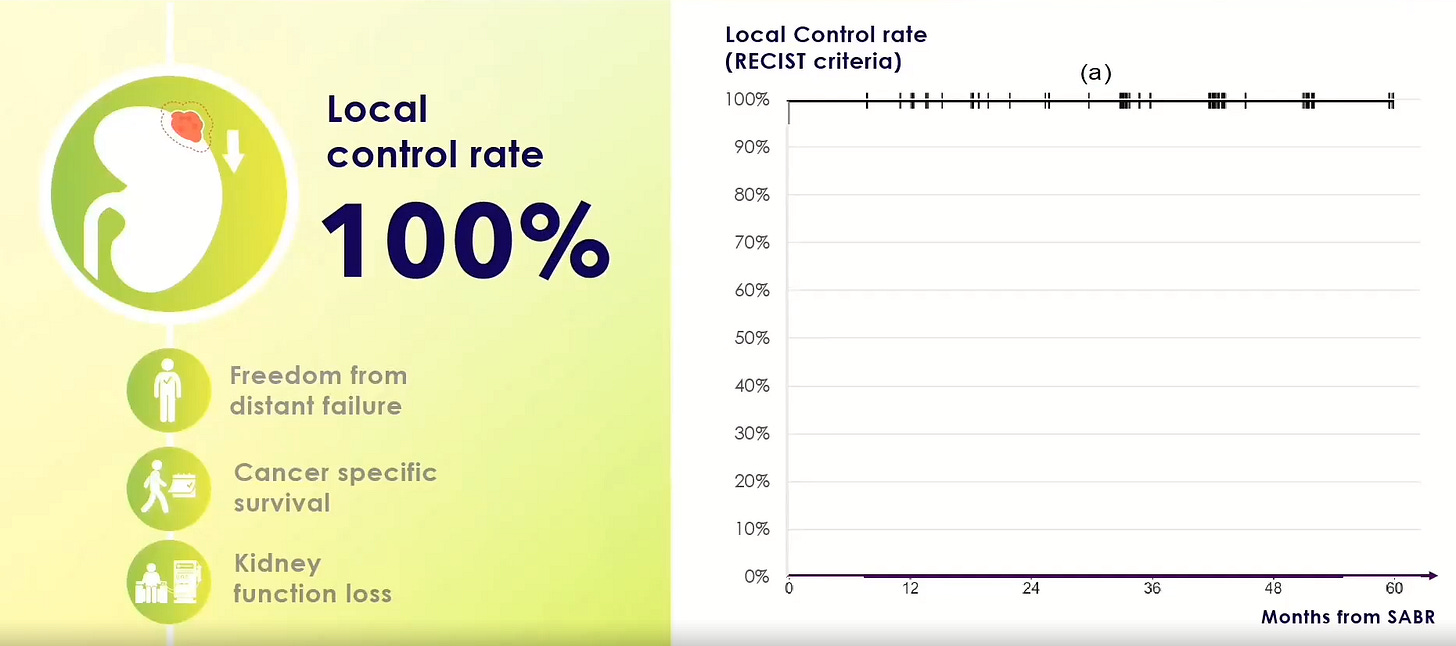
100% local control, no one passed away from renal cancer.
Median follow-up at report is 43 months.
Freedom from Distant Failure was 99% at 3 years and 92% at 5 years.
(so two apparent failures - one at approximately 6 months and one at approximately 50 months).
And importantly:
Cancer specific Survival was 100% at 5 years.
Kidney function did decline which is certainly expected, after all, the tumor is in the kidney. That said, the average loss was 14.6 mls/min. In the trial, one patient with 5.9cm central tumor with baseline function of 34 mls/min did require dialysis.
Beyond the kidney direct effects, there were no Grade 4 or 5 toxicities. There were 7 (10%) Grade 3 toxicities. The most common toxicities were transient pain (3%) or nausea vomiting (4%). Prophylactic antiemetics or steroids were not mandated, but should be considered based on the slides from the presentation.
Here is the summary slide while we wait for the publication of the data.
Simply a big win for the specialty and for our patients. Maybe not a surgery replacement today but certainly supports this as a strong alternative approach. And yes, it is a rather small study, but when paired the work below, it appears quite valid:
5-year outcomes after stereotactic ablative body radiotherapy for primary renal cell carcinoma: an individual patient data meta-analysis from IROCK (the International Radiosurgery Consortium of the Kidney)
This work was published in Lancet last year, and when taken in totality, I think you can begin to make a very strong case that this approach is a clear and valid option as a standard of care option for many patients with renal cell cancer.
Here is another statement from experts arguing that it does make sense to support the use of this approach - note published well in advance of this recent trial presentation:
The Judicious Use of Stereotactic Ablative Radiotherapy in the Primary Management of Localized Renal Cell Carcinoma
Here is a portion of the conclusions from this review article from July 2023:
Finally: It is Consistent with our Literature.
The Broader Context:
As I’ve said before, SBRT approaches - ablative / tumor killing doses of radiation to (generally) smaller targets via shorter fractionation has been the biggest pathway to progress in the last 20 years. It has replaced “IMRT” as our fields largest technical breakthrough during this time period in my assessment.
In just this year alone, I have written about outstanding results in lung cancer - where it appears that radiation can substitute for surgery. The study out of MD Anderson showed great results using tumor killing doses of radiation paired with a short course of immunotherapy - not years, but 12 weeks of immunotherapy - summarized here:
A Major Synergistic Win In Lung Cancer!! High Dose Radiation Plus Immunotherapy
And I’ve written about the use of high dose proton therapy and SBRT photon approaches being superior to radiology procedures like TACE for liver cancer. In liver, as the data grows, to me, it is quite clear that high dose radiation outperforms the most common interventional radiology procedures.
Randomized Prospective Trial Demonstrates Proton Therapy Outperforms TACE in Liver Cancer
And then recently, we’ve demonstrated 96% control for prostate cancer in intermediate risk disease - a mark that cryotherapy or HIFU simply can’t touch. In fact, the results are so strong that surgery would have a difficult time hitting that disease control mark - and this discounts the toxicity differences seen in PACE A.
PACE B: 95% Cure Rate at 5 yrs!!
And now we demonstrate progress again in high risk non-surgical patients with renal cell cancer! It is amazingly consistent with what we are seeing in lung, liver, and prostate. Radiation is simply a great non-invasive curative treatment. Our shift to smaller targets, eliminating or minimizing normal tissue treated, and shortening our approaches have allowed for dose escalation and allowed us to cure more patients.
A Look Back:
Back in the day, we called the first high dose radiation approaches SRS - it started in the brain but, to me, the wording was really pretty good - Stereotactic Radio Surgery.
The goal was pretty simple - explain to others that this was using radiation more like surgery.
Somewhere along the way, people got names on publications for moving away from that language to SBRT or SAbR. We got “fancier” and added one letter (sometimes capitalizing them all - other times, not), but dropped something pretty important maybe to the broader audience - our patients and referring physicians. We dropped the word “surgery”. It’s important to remember that these approaches really do begin to mirror surgery only - doing it without an incision. And yes, maybe “ablative” is “more accurate” but really? How many patients know that word compared to “surgery”. Heck, even if I asked radiation oncologists what is an “ablative” dose, the answer would be quite nuanced and depend on number of fractions, histology, etc. We don’t even precisely know what it means. Surgery simply means to many - get rid of it.
Looking back, I’m not really sure I agree with that shift. In a way, it is really a rather poor move in our self-advertising. Arguably maybe we made it “more accurate” but we also made it more obtuse and difficult to simply explain to patients and referrings in the new “improved” acronym. Pretty sure most marketing agencies would have vetoed that shift. I digress…
If you back up to the late 1990’s, both renal cell and liver cancer were considered radioresistant. Or at least that is what I was taught. We simply didn’t treat these diseases. Not sure I treated a single case - or more precisely - I don’t believe I remember seeing a single presentation of a single definitive case in my 4 years at MD Anderson (back in the day, we presented every single definitive case to all staff and residents in a big single morning meeting). So either my memory is quite poor or these were, at least, very rarely treated diseases.
Now fast-forward to 2023, where I think we have used great technology - both in the machines that deliver treatment and in the imaging and software that allow us to deliver really high tumor destroying doses to the tumor while sparing the nearby adjacent tissue. Turns out maybe they weren’t “radio-resistant”, maybe we just didn’t have knowledge and tools to get them treated safely to the dose they needed back then.
And at the same time, with shorter and more effective treatments we continue to make strides towards increasing our use-case against surgery. Perhaps moving towards reserving surgery for the times we cause damage that won’t heal (a story for a different day). Renal cell is an excellent example. It is completely consistent with our experience in lung cancer and prostate cancer where 5 fraction or fewer approaches are competing with - or exceeding the outcomes (tumor control and toxicity profile) in three diseases.
And relative to TACE or Cryo or other radiology type approaches, this data is again supported by broader context. Simply substitute liver for lung and make the same arguments. In liver, prostate, and now renal cell cancer, we are demonstrating clear data that radiation is an excellent option - often with simply superior cancer outcomes than these alternate procedures that attempt “ablative” approaches.
And as we go, remember that renal cell is a big indication. It is the 9th most common cancer worldwide - increasing incidence - especially in those over 70 and as this slide demonstrates, this choice checks a lot of boxes.
Sometimes short definitive approaches are best. We’ll take that theme to today’s discussion and stop here. A clear definitive win. Kudos to Dr. Siva and all the study participants - great work!! Hopefully my quote / memory of the evening wasn’t too affected by the wine.
Thanks, as always, for following along as we search for better. Excited for the next few - a story of sorts guaranteed to educate on how you approach high dose, short course, surgery-like radiation and a look at radiation once again demonstrating big benefit to patients with metastatic disease.
If you made it this far, consider hitting the like button. It really does help me out and it takes less time than it took me to put this together - guaranteed.











Great post. I love your focus on emphasizing the value we’re delivering to patients and the health care economy overall. We’re an extremely cost effective modality that can cure cancer without incisions. That is the drum we should be beating.