Randomized Prospective Trial Demonstrates Proton Therapy Outperforms TACE in Liver Cancer
How Proton Therapy Reshapes Hepatocellular Cancer treatment improving outcomes and lowering costs.
Yep, that is correct. Proton therapy appears to clearly outperform TACE for hepatocellular cancer in a randomized prospective setting. And it wins on outcomes to such a degree that cost of care becomes a clear victory as well in favor of the radiation oncology approach. Yay!! Nice to see a clear radiation victory.
And yet, within the first 24 hours of demonstrating that proton therapy is far more cost effective than the current most common “standard of care” approach. We - radiation oncologists - seem to want to tear down our successes from the inside. Seriously, you can’t make this content up and I guess in odd ways, fortunately? for me, I don’t have to.
To me the first question is quite appropriate. “Does it have to be proton therapy?”
But the second statement is laughable. The study literally demonstrates that protons are LESS costly than the most common “standard of care” option and yet we - as radiation oncologist - immediately use the term “financial toxicity” referencing our own value. And we wonder why we struggle? We wonder why the bad press and negative slants in journals regarding important recent studies? Yet, often, all we need to do is look in the mirror and consider just how often we lack a unified supportive voice for our field which provides incredible value to cancer patients. Opinion of one.
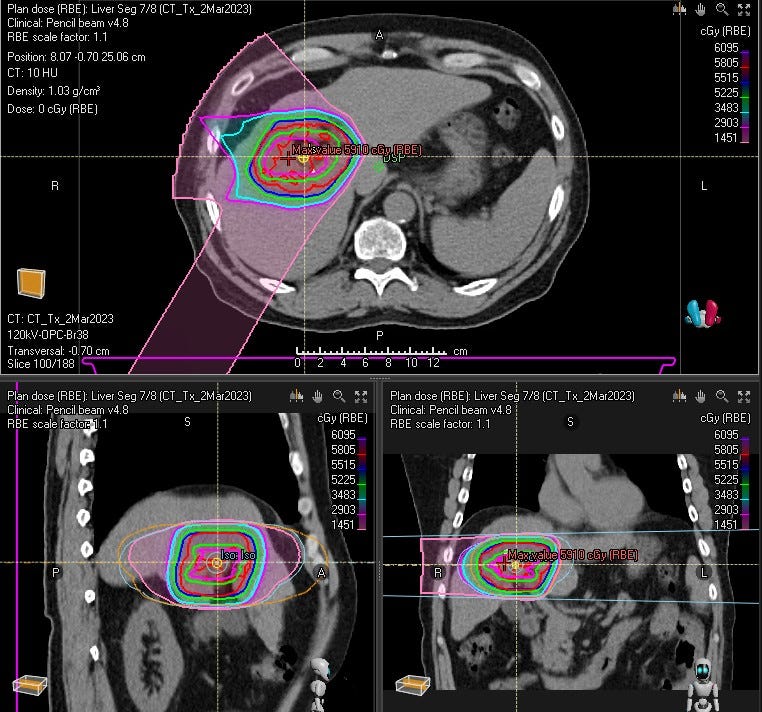
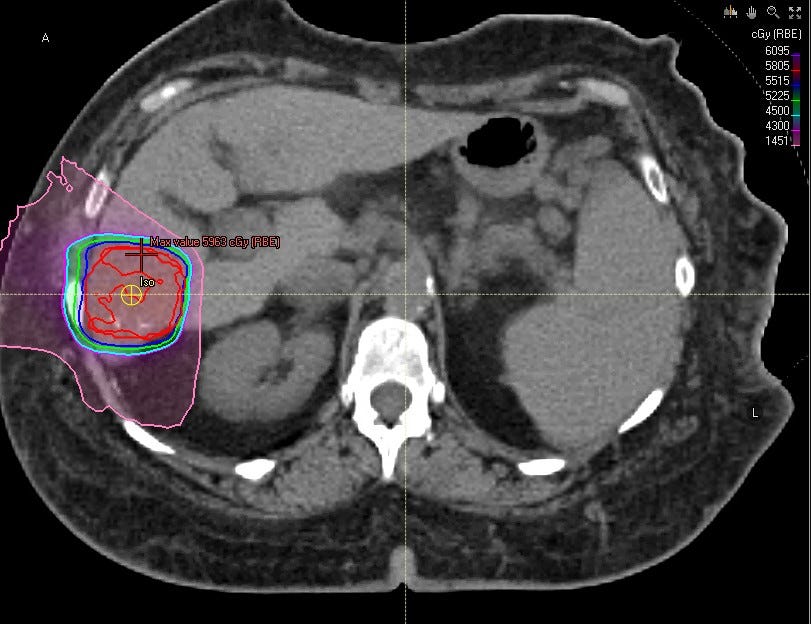
Today we’ll focus on the study and present several example cases, attempting to address the former question. That really is our focus, attempt to describe differences using cases. Hopefully by showing pictures people (surgeons, medical oncologists, radiation oncologists, even patients) can quickly get a feel for different types of cases and when protons might make the most sense. I really do think this should shift standard of care options towards greater utilization of radiation and more specifically, proton therapy in the treatment of hepatocellular carcinoma. Kudos to the authors for their work in getting this trial done - these have been very difficult to do!
The Randomized Prospective Trial:
Note: the trial has clear limitations. It is small and follow-up seems rather limited and arguably less than one would expect. Further overall survival, the primary endpoint, was equivalent. Those are clearly the downsides to this, but I still believe this is simply a win. As always, you decide.
Methods and Objectives:
Subjects were randomized to receive PBT (n = 36) or TACE (n = 40). Proton therapy was administered in 15 fractions over 3 weeks to a total dose of 70.2 Gy. TACE was repeated until complete or maximal response. The primary outcome measure was overall survival (OS). Secondary end points were progression-free survival (PFS), local control (LC), toxicity, and cost.
Mean tumor size was 3.23 with about 37% having tumor sizes between 3 and 5 cm and 12% larger than 5 cm.
A comment on protons vs. photons in general for liver cancer: the proton beam approach is simply different than a photon approach and we’ll get to why / how below but the dose given was 70.2 Gy / 15 fractions - so 4.68 Gy(RBE 1.1) per fraction with 1cm margins around obvious / visible disease. Most photon approaches will be to a lower - often quite lower EQD2(10) dose with tighter margins - so different dosing, different targets, using different fractionation approaches.
Remember: OS was the primary outcome measure so this is technically a negative trial but protons win on local control with a hazard rate of 5.64. Generally I’d argue against using secondary outcomes - but read the paper - look at the benefits and ask if it is a win? I think it clearly is: Protons win with a large reduction in hospitalizations. Protons win in requiring fewer downstream retreatment procedures and via all those wins, they win on cost despite being between 4-5k more expensive upfront.
Here is the strongest curve in my assessment showing a strong difference in progression free survival in favor of Proton Therapy.

And they win on toxicity at lower grades with wins in abdominal pain (p<0.001), nausea (p=0.05), fatigue (p<0.01), and total bilirubin (p<0.01).
Again, if it falls apart it is in follow-up length and patient numbers and arguments for it not demonstrating an OS benefit. But a lot less hospitalization and repeat procedures, in a very real way, means more good days out of the hospital - a very important clinically relevant metric for this disease when mean survival is unfortunately 32 months.
And from a radiation oncology perspective, this continues to strengthen the argument that radiation outperforms TACE or RFA approaches achieving high control (REF 1, REF 2, REF 3). So as a specialty, I haven’t seen many really questioning the general trend of the conclusions.
Well, aside from questioning: “yea, but I mean, I could do this with photons. Right?”
But, here, for this disease this question of “can I do this with photons” gets back to the very different historical approaches in the proton world compared to the photon world. This is one of the most divergent sites in our entire specialty with respect to approaches. Simply stated, for decades we didn’t treat liver cancer due to toxicity / inability to deliver good dose and avoid liver, bowel etc. At my time at MD Anderson (1997-2001), I remember treating far more ocular lymphomas than hepatocellular cancers - it just wasn’t done due to real toxicity issues.
In more recent years, SBRT has stepped in and helped make traditional photon treatment a viable alternative, but doses still often lag behind protons. And let’s be clear: If the approach in this study was to the same dose with similar margins, I have ZERO doubt that this would be globalized to photons immediately - whether that is correct or not. The impact of integral dose differences would be assumed to be near zero impact. Here, the only reason for the pause is the difference in both margin / dose that makes even pretty strongly leaning physicians in favor of photons question that translation.
Pandora’s Box Begins to Rattle
I discussed this previously in my “Why We Require Randomized Data for Protons”, there are real ramifications to our field as we attempt to prove one radiation technology is superior to another.
And this really becomes the question - like in the MRiLinac MIRAGE Prostate Study (my summary article on the MIRAGE Trial here) - was it technology or was it margin? Is it protons and limiting the volume of liver and bowel treated to lower doses or was it the dose escalation? Can photons just do something using SBRT approaches and maybe accomplish pretty similar results - perhaps with much tighter margins and with doses that are often less ( at times 30%-40% less) than in the photon world, but maybe are close enough to achieve 80%-90% of the local control that higher doses obtain. Here, the photon argument pretty quickly slides to a “good enough” argument with a number of “maybes” or “perhaps” required - at least until the randomized data is available comparing photons to protons.
As someone who has grappled with the opposite side of this question from a “lack of randomized data” setting repeatedly now for almost half a decade, it is quite a different perspective to see the debate on benefit be flipped somewhat on its head.
But rather than rehash data or look to try and make some detailed analysis of small trials and complex comparisons via retrospective comparisons, I’d just say simply:
There’s more data supporting protons in liver cancer than most other sites - it is a Tier 1 ASTRO recommendation based on this data. (Example ref)
Historical dosing for protons treating HCC is simply higher than photon approaches have been historically.
The ideal answer will be in about 6 years when we have results from the NRG randomized trial.
And with those rather broad statements, I’ll jump into something more reasonable to me: let’s look at some example cases and I think most will see that there is real potential where differences in approach very likely might benefit a proton therapy approach and therefore likely represents a real improvement in outcome.
My initial plan was to run a few comparative plans and so I opened up our database and starting running through 2-3 dozen HCC cases treated over the past 2 years or so and visually I started seeing patterns. And those patterns, to me, illustrate the point better than a handful of multi-plan optimizations. So today we’ll kind of look at a few pictorial examples.
Obvious winners and less obvious cases:
Ok - so context. I think protons make life much easier when you treat HCC. You get to treat with higher doses with rather extensive safe clinical historical data and the fall off low dose regions are dramatically better - at least for many cases.
At our center, we tend to ONLY see the ones that IR won’t touch or where they are hesitant. Even at a proton center, getting these patients out of the IR factory is very difficult. So I don’t have many small volume or multiple smaller site examples. They are mainly larger volume lesions or central regions of the liver but I think they still illustrate benefits.
Hopefully after seeing some images people might better pick which patients might benefit the most. That is the goal. And yes, these are USPT plans - PBS would enable more shaping of the high dose region to the PTV in places.
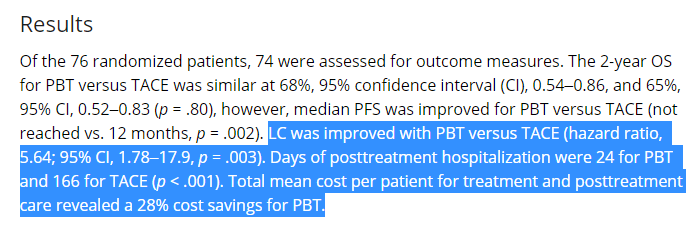
Scenario 1: Posterior large volume peripheral lesions
To me these are wins for protons. Large volume, little to no significant lung volume changing posterior to the lesion. From 45 BED to even 80-90 BED, little changes. Add dose, nothing changes. Liver doses, bowel doses - ok maybe rib fracture risk but realistically, with photons there is a balance - higher doses generate extra dose beyond target. Here there isn’t a compromise and protons simply have good data up to 60 -70 Gy in 15 fractions. EQD2 dose approaching 75-85 in a large lesion. And we’ve seen no reason to back down. This is one group where I like considering protons strongly.
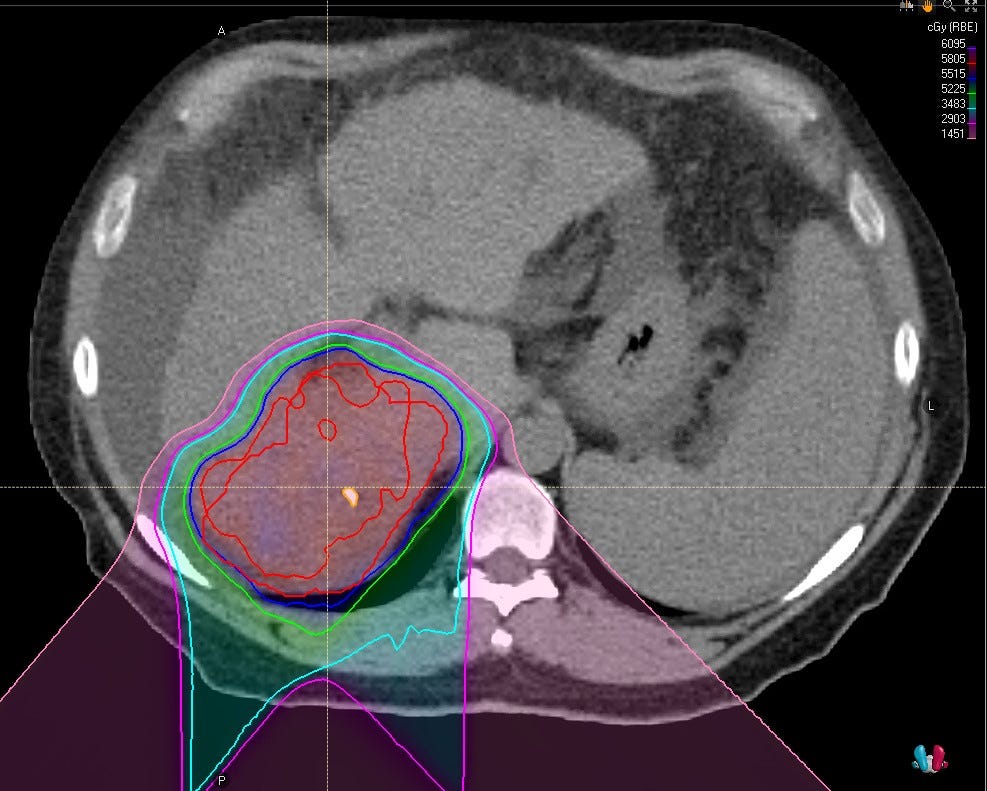
Scenario 2: Anterior or lateral large volume peripheral lesions
Same arguments in favor (just need to watch the tissue / lung interface difference through the respiratory cycle) especially as you get higher in the liver. In my experience, protons still win pretty easily and consistently but the more lung variance from inspiration to expiration you see, the more range effects matter which must be considered in the planning process. The more stable or less lung interface, the easier the win for protons.
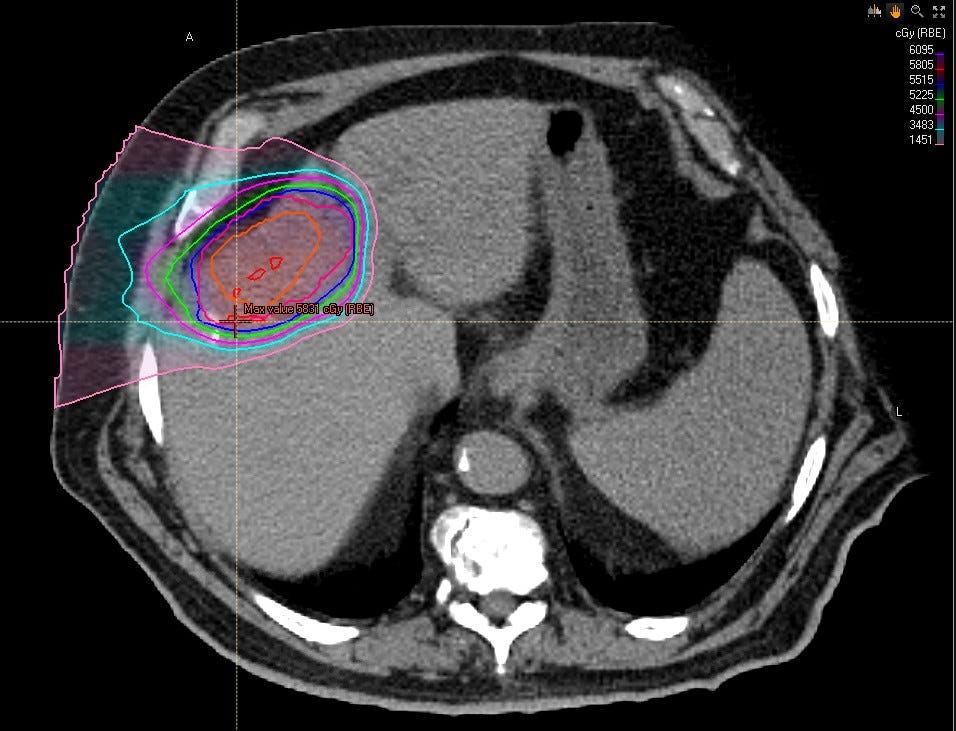
Scenario 3: Large central lesions
Here, in our clinic we’ll often reduce the dose to 58 / 15 for these large central lesions where you really worry about bowel doses. In the study they treated to 37.4 Gy(RBE) in 8 fractions and then made a reduction and continued with the additional disease to the same 70 Gy mark limiting bowel dose to 50% for the remaining 7 fractions.
So max bowel dose was 76% of script: ~53% (8/15) + 1/2 of 47%. So 53.35 Gy was max bowel surface dose - so an EQD2 (10) of 60.23 Gy. So in a photon world about 40 Gy / 5 is the minimum photon dosing for this cohort because most treat via SBRT type approaches. I believe that would still be considered quite high dose for many programs with many backing off significantly from there to 30Gy or down into the upper 20s.
We’ll typically make a reduction around a similar time and then continue to 58 in 15 with tight volume constraints on the bowel. This is still a dose of 67 Gy BED10 so often 50% higher than what is delivered in the photon world. But more of a compromise as we near bowel structures - albeit still quite a bit of dose. And realistically after publication of this data, we likely need to push a bit higher and be one more step aggressive even in these cases.
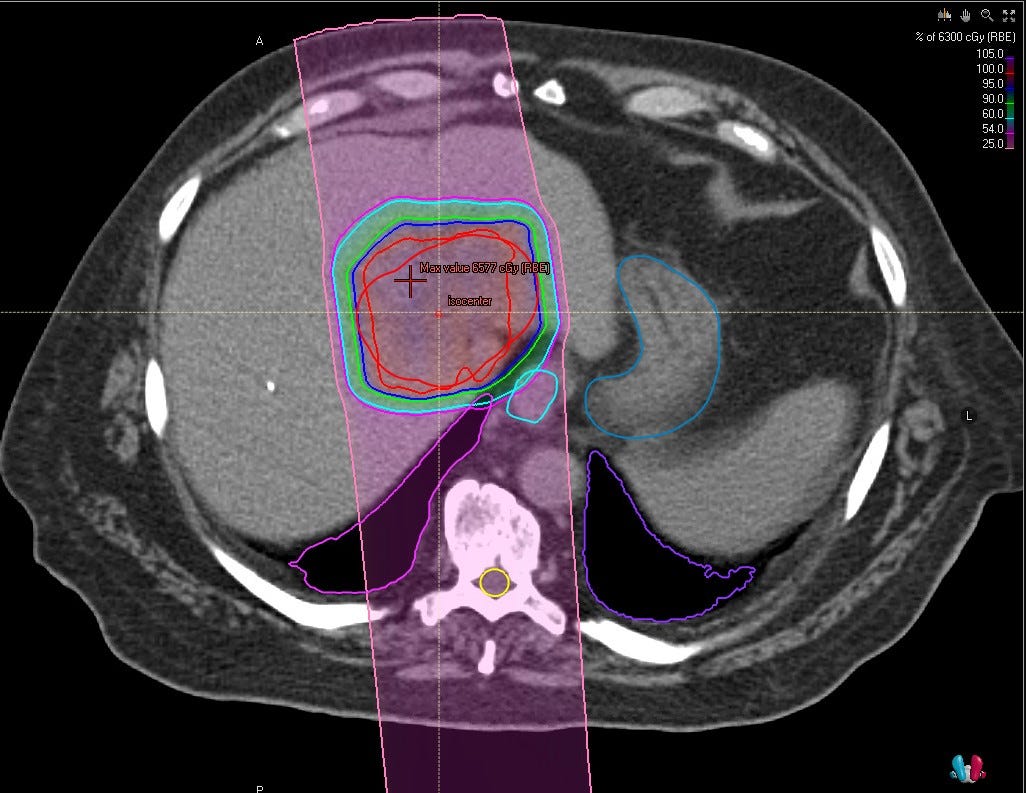
Scenario 4: Smaller lesions
The gap to photons is perhaps less as these are easier to treat with photons, but dose is still quite different. But in smaller lesions, dose might matters less and SBRT dose appears reasonable (based on retrospective local control publications). That said, proton dose is still generally higher and to me, the onus now falls on photons to prove the dose differences don’t matter or demonstrate a narrowing of the dose gap can be done safely.
Is Dose “Escalation” Really Required?
Which is a funny question in ways - it is our entire argument against this radiology / intervention space - we give more consistent dose to all the tumor. And so while I understand the question and it is scientifically quite valid and quite appropriate, it lands a bit crooked in this space from my perspective now 4.5 years after arriving in a proton facility.
Because today, looking at Yttrium-90, we dismiss the super high point doses and focus on our ability to give nice uniform dose across the entirety of disease. Does the benefit start to shrink with more and more dose once you hit some point? Almost certainly. But in the images above, you can see that with protons there are many cases where the extra dose doesn’t affect much of anything beyond the tumor. The dose escalation with protons is often largely “free”. In photons, increasing the BED10 from 45 to 85 will drastically change the adjacent normal liver dosing. In contrast, stopping a proton plan early has minimal improvement in normal tissue dose - especially in the more peripheral cases as illustrated above.
To me, it’s not really dose-escalation here. The question is really, more accurately stated, can dose-de-escalation with photons achieve similar results.
The Phase II Trendy trial is arguably one of the stronger ones in the photon space. It used 8-9Gy delivered in 6 fractions out of the Netherlands. That is troublesome for the US market as it doesn’t hit our magical “5” fraction SBRT definition. It gives more dose (72 Gy - 85 Gy EQD2(10)), but doesn’t fit our market’s coding requirements. SBRT dosing per NCCN is 30-50 Gy in 3-5 fractions. Some of those compete with these proton approaches and some would be 1/2 the dose.
There is a highly cited study by Bujold which ultimately points towards lower doses being quite effective in HCC which adds value to the dose question. But I think we all acknowledge the uncertainty and lack of precision in these types of regressions.
In Summary:
Protons have a long track record of safety and limited toxicity treating liver cancer to these doses. We now have randomized prospective data showing benefit when using high dose proton radiation delivered to the whole target when compared against, arguably what was the Standard of Care treatment in TACE.
And, so to me, the proof should move to IMRT to demonstrate that lower doses / tighter margins / extra integral dose doesn’t matter - where machines outnumber proton installations 100:1, one can argue the accumulating the data should come quickly. The fact that this hasn’t been performed to date, in and of itself, speaks to the difficulty we’ve historically had treating this disease with photons. That difficulty / hesitancy opened the door for these alternative interventional radiology approaches into this space.
Let me be clear, I think SBRT with photons is currently just better than interventional approaches for most cases but I’m a radiation oncologist. I also think, likely by about the same ratio, protons allow for easier, safer treatment today compared to photons for many of these lesions. I think this stepwise assessment of options is generally supported and consistent with a growing segment of the medical literature.
And with the help of pictures, maybe some physicians now better understand the lack of compromise for many of these cancers when treating with protons. For many cases, there is little drawback for significant dose increases.
Ethical Issues Resurface:
A quick closing thought.
Two clinic settings:
One in a region with no protons and a second where a “competing” facility sits just down the road with proton therapy available. Each now is interested to run a randomized trial comparing SBRT to TACE to prove their ability to reproduce these results.
To me, one trial is quite ethical and one is now perhaps less so. Especially until the randomized trial comparing protons and photons is completed. These are real issues that we need to be attempting to address prior to the coming of age of so many well designed randomized comparisons.
And that is the rattling of Pandora’s box as we move forward on the path for better.