Why we require randomized data for protons.
In the past, some in leadership actually argued against this approach. With greater time and more hindsight, I'll try to discuss why this data is critical to the industry.
www.protons101.com
Home to the musings of a radiation oncologist - with a slant on protons and dose and optimizing cancer outcomes.
“They’re just plain better and you don’t need clinical trials to prove it.”
I remember sitting in our morning conference when this statement was made back in January of 1999. Jarring enough to write it down then and still jarring enough to remember the quote / card today. MD Anderson was looking at how to build and fund their original proton center and was bringing in experts to develop a path forward. I was in training - a fly on the wall so to speak. Interesting times.
And let’s be clear, it wasn’t a passing quote taken out of context. Dr. Suit in fact wrote an editorial in the JCO in 2008, nearly 10 years later, which was supported by Dr. Cox. There was, of course, an opposing view both then and now, but today we’ll look back at this piece of our history.
After all, history is important. Often, and sometimes correctly, we assume we have adjusted for old errors, but maybe just as often we assume things are different when they are not. From medicine, to politics, to business: patterns repeat. Today we’ll look back at two components of our history that are often ignored / forgotten / not mentioned when we examine the current proton industry. In fact, a recent talk this past weekend on our troubles generating randomized data didn’t address either point. I came away from this journey remembering quite a bit and learning even more. Hopefully you find it interesting as well.
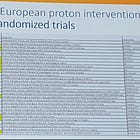
Last week I purposefully included a list of ongoing European randomized studies (link below) - as I’ve said, the data are coming, but today, a look back:
History Notes: Suit (Mass General - ASTRO Gold Medal 1990), Cox (MDACC - Gold Medal 1994), Peters (Emeritus - Gold Medal 2003) amongst others. Pretty crazy historical list we will cover - privileged to have had a beer with each of them over the decades. Each of these leaders of our field did wonderful work for our specialty. Decades of dedication. Kudos to each of them for the work they did to push our field forward!!
But I do think this old debate lies near the center of many radiation cost discussions today. And so, we dive in - it is after all, our history.
Two Historical Editorials:
Dr. Suit penned this Special Communication in the green journal in 2008:
Pretty straightforward - enough for the title to suffice:
No, Not needed.
So clearly my radiation oncology boards review card, the one above where I jotted down the quote due to my surprise at the position, was not incorrect. Nearly a decade later we continue the same provocative stance and simply argue that we know enough to move forward without them. The dosimetry plan differences alone justify use.
And along with that article came this editorial commentary by Dr. Cox who served as the Chairman of the MDACC program during my training:
Should randomized clinical trials be required for proton radiotherapy?
Just for flavor, a few quotes:
It is therefore hard to imagine how any objective person could avoid the conclusion that there is, at the very least, a high probability that protons can provide superior therapy to that possible with x-rays in almost all circumstances. It is primarily for this reason that the practitioners of proton beam therapy have found it ethically unacceptable to conduct RCTs comparing protons with x-rays.
Of course, it is really all about money. Can anyone seriously believe that, if protons were cheaper that x-rays, there would be similar objections raised as to their immediate and widespread use? This seemingly rigorous academic discussion, in reality, is driven by the uncontested fact that protons are more expensive than x-rays.
We doubt that many of us, while healthy, would agree to receive, for example, 25 Gy to a large fraction of our brain or abdomen in exchange for some thousands of dollars, with no known or credibly hypothesized medical benefit. If we would not, how can we ask our sick patients to do so?
Then, as now, there were arguments to the contrary but I do think it is important to understand that this was from leadership. Leaders of some of the largest institutions - like that or not - that is our history.
There was and is a counter voice. To me, the best science comes from good discussions - arguing both sides so that people have full context of the perspectives. It is what allows to build good studies and press knowledge forward.
As an example of the opposing view, here is a 2010 article arguing against that approach. And it really focuses on the cost issue and pushes back on that part of the debate.
Technology Evolution: Is It Survival of the Fittest? (Tepper - UNC Gold Medal 2008, Zietman - Mass General Gold Medal 2016)
We judge that the truth lies somewhere between these extremes.
We think that there are some situations in which protons are probably not superior in the present state of the technology, and acknowledge that there are technical aspects of proton therapy which, if not properly taken into account, could lead to inferior results.
Hospital administrations must accept that a technology should neither be used for prestige nor for marketing, and their business models should be based on conservative, rather than optimistic, assumptions about patient accrual. The value of proton therapy is not a slam dunk, but large advertisements give a different impression.
There is widespread agreement that the seemingly inexorable rise in health-care costs needs to be curbed. It is our view that, rather than imposing rationing, the issue is better framed in terms of curtailing the use of those technologies and procedures that are of minimal additional benefit to the patient in the interests of preserving funds for approaches that are of real value.
And there you see it. The creep to what became “Choosing Wisely”. Paired with IMRT expansion, these two issues sit at the center of the path we opted to take around this period.
(Again, today, as I’ve discussed, we are a drop in bucket - overrun by pharma, but here you can see the divide beginning to form and an emphasis on our internal cost structures).
To me, what is more surprising about the argument AGAINST randomized data - is our history. If you back up, you see we messed up before.
Please comment below or if you know the history better than I describe or care to add insight.
Fast-Neutrons: All but gone today.
Fast neutron therapy - due to complexity and oversimplification of RBE is now nearly gone from the earth - 2 facilities today so far less than carbon. Here is a look back at that segment of our history.
An interesting 17 page paper regarding Relative Biological Effectiveness (RBE) - published in 2001 by among others, Lester Peters.
The effectiveness of photon beams varies much more markedly with the dose rate than the effectiveness of fast neutrons.
RBE is a dose-dependent parameter, generally increasing at lower doses. For this reason the clinical RBE has also been assumed to increase as the dose per fraction is reduced.
RBE will vary among studies depending on the reference photon beam used. The original reference was 250 kVp but as of 2001 is usually Co60.
Cyclotrons with similar accelerating energies cannot be assumed to have the same RBE. For example the Clatterbridge(UK) were 5% “less effective” than the neutrons at MD Anderson.
The main point here is RBE is complex. Far more complex than many likely appreciate. And while neutrons are a high LET form of radiation and protons are a low LET form of radiation (similar to photons, electrons), protons have complexity in their dose deposition especially near end of range that make them have some features of both low and high LET radiation.
Here is a second paper from 1981 discussing our neutron experience.
Fast neutron therapy was initially condemned because of a report that its use resulted in excess late normal tissue damage (statement is a reference from a 1948 article).
Today (1981) there is danger of repeating the mistake by paying insufficient attention to the basic radiation biology. This is most notably demonstrated in the use of a single RBE of 3.0 for all tissues and for a wide range of treatment regimes in which different dose/fractions are used.
The general clinical use of an RBE of 3 for neutrons is shown to be not only incorrect but also dangerous. RBE is dependent on the dose/fraction of either photons or neutrons and differs for different tissues.
The RBE for the CNS is contrasted with that for skin damage; at a photon dose/fraction of 180 rad, the RBE for the CNS is about 5.3, compared with about 4.3 for skin damage.
We have attempted to illustrate the danger of using a single RBE of 3 by examining the clinical results of spinal cord irradiation. This is only one example of a general problem. RBE is not the same for different doses per fraction and it also differs for different normal tissues and, of course. also for different tumors
When I arrived at MD Anderson, the neutron program had closed. I looked for studies or for the rationale online and couldn’t find anything as the internet didn’t exist back then and I didn’t head to the library. I have a story in my head, but uncorroborated, I won’t just type it. But pretty certain it was primarily toxicity issues. And due to this toxicity concern (at a minimum) as well as difficulty in collimation and modulation of the beam, there are only two operational sites today in the world.
Simply too complex. Too large of a leap from photons and ultimately, and so on some simplistic level, we swapped over to protons in our research and in our push for better and to hopefully avoid toxicity issues.
RBE / LET for Protons
But in a similar light, we knew we had questions regarding a translation of dose between photons and protons. I’ll give some references. You can go and evaluate for yourself, but it is actually some of the same authors arguing very strongly in favor of proton therapy that comment on the complexities and uncertainties. And what is more confusing to me is the era of the poor / “less than ideal” neutron results overlaps with the era these physicians practiced. So it wasn’t like they were not aware of the neutron issue.
Just for context, here is a paper from 2002 clearly discussing a lack of certainty regarding RBE at the distal range of the beam.
Relative biological effectiveness (RBE) values for proton beam therapy
The average value at mid SOBP (Spread Out Bragg Peak) over all dose levels is approximately 1.2, ranging from 0.9 to 2.1. The average RBE value at mid SOBP in vivo is approximately 1.1, ranging from 0.7 to 1.6.
The experimental in vivo and clinical data indicate that continued employment of a generic RBE value and for that value to be 1.1 is reasonable. However, there is a local "hot region" over the terminal few millimeters of the SOBP and an extension of the biologically effective range.
So we knew it was a possibility - a lack of clear precision of dose at the end of beam. And it is part of literature - a clear understanding for these complexities that appear to have fallen to way side in the editorial articles above - both in favor of not performing trials and the in the opposing view arguing for the their need.
Here is our “definitive” current physics document on the topic:
It discusses RBE and LET issues at length. Here are a few quotes. Again, there are literally pages of this type of discussion in the document:
Although there is a large amount of data on the RBE for clinically relevant LETd values, (α/β) γ and doses, the proton RBE values are still associated with considerable uncertainties.
RBE increases with increasing LET and thus with increasing depth if an SOBP is being delivered.
These average values consider 2 Gy at the point of interest. There is also likely an RBE increase as dose increases in the distal as well as lateral fall‐offs.
Caution is warranted for small SOBP widths (and tumor targets) and/or low (α/β) γ where the average RBE could be higher.
There appears to be a slight trend toward an increase in RBE as (α/β) γ decreases.
An aspect that needs to be considered is the move toward scanning beams, which may result in overall slightly higher LETd values compared to passive scattering. Whether this will impact an average RBE is unclear.
Or a good quote from just this past weekend:
Proton cGy(RBE) modelling is not a high precision science (we know the age of the universe with a lot better precision!) Erik Traneus, Raystion LET/RBE expert.
And finally, a pre-release version of RayStation incorporates sliders that allow you to manipulate “clean” (low-LET regions) vs. “dirty” (high-LET regions) dose - essentially adding a mechanism to better model this uncertainty.
My point is this:
Without question there remains uncertainty - more than with photon treatments. We continue to work towards the best path to integrate that greater uncertainty into our dose modeling and plans.
Understand I think the effects of any difference are quite minimal - primarily due to the rapidly expanding clinical experience, but it is unwise to ignore this physical trait of protons. In fact today, we might see this used to potentially improve cell kill with protons over photons. One can make arguments for both higher potential cure and/or higher possibly toxicity. But again, this potential difference is something one must consider and should not dismiss.
I file it next to alpha / beta calculation in SBRT - we’re likely close but remember the uncertainty when you read trials / assess data. And this is not new. This has been known for at least 40 years.
My Summary of this History:
I take away a few things from these articles - cyclotrons and higher than photon LET work has been part of radiation oncology for ~80 years. Today we are focused on protons and carbon but it is important to acknowledge they are a significant component of our history.
Secondly, there are true complexities that must be considered when we move from photons to other radiation forms and that persist even in a transition from passive scanning to pencil beam scanning approaches. I think there is good work on LET (which can be calculated) as a tool to predict / minimize RBE deviations (that is my one sentence version of a vary complex topic).
Today, we often look past these two issues - one of history and one of physical uncertainty - but each are important.
From my perspective reviewing history is critical. It gives context as to where we are today and can help us to be more efficient in our efforts to move forward. These are complex issues and will require bright minds, hard work, and a great understanding of our history to prove these approaches beneficial.
With that in context, what has changed since about 2008 that maybe gives us more clarity today than we had back in that time period.
Well, for one, the Lung Cancer Trial:
You know, this one.
The one where we looked at protons vs. photons and ah… if anything Grade 3 toxicity trended against protons. Sure we can parse and look for rationale (passive scanning / lung tissue interface / dosing etc.), but all must agree it was NOT a win for protons.
Note: Dr. Cox is an author on this trial. So while you might disagree with his earlier stance, he is an author on arguably the biggest trial demonstrating a lack of value for the industry. I think it demonstrates a humility in attempting to follow the data amongst these leaders that is, my opinion, too often lacking in medicine today more broadly.
Today, we have the Esophageal trial that to me, does clearly demonstrate less toxicity with protons, but it required complex metrics - to say it is a slam dunk clear win is a bit of a stretch. I think it demonstrates a win, but hard fought in an ever changing world.
Further IMRT has had a tremendous cycle of improvements - VMAT, non-coplanar SBRT, image guided improvements and iteration across thousands of machines and clinics - not just 20 or 30. In the end, it has made chasing down this progress - to date - not clearly demonstrable.
So we have 1) uncertainty and 2) a lack of easy wins. And within that context consider
A Twitter Conversation on Nasopharynx treatment approaches:
Here are some quotes taken from the longer thread:
James Caudell, @JJCaudell (Moffit HN): Had more than a few CNs (partic XII) drop out late (5 years+) with 210-212. Switched to 200/d a few years ago.
C. Jillian Tsai, MD, PhD, @CJTsaiMDPhD (MSKCC HN): Honestly I think 6996/7000 are very similar - key is to scrutinize where the hotspots are & to avoid hotspots in critical structures. I've also learned that institutions evaluate plans very differently, some look at 100% IDL and allow higher hotspots and others evaluate 95% IDL.
David Sher, @DavidSherMD (UTSW HN): I generally still do 6996/33 for NPC - mostly out of habit - but pay an obsessive amount of attention to heterogeneity in the PTV6996. Ultimately it’s 5% hotter per fraction, by definition, and that could mean something in the wrong place.
Daniel Ma, @DanielMaMD (Mayo HN): We have a lot of intracranial extension, Meckel's / cav sinus involvement with our pt population, so we've usually used 35 fxns to keep each fraction a tad cooler.
𝖉𝖆𝖛𝖊 𝖋𝖚𝖑𝖑𝖊𝖗, @cd_fuller (MDACC HN): christian roenn working on this; example: RTOG and ICRU prescriptions can mean “prescribed dose” is vastly different between plans that may be similar (and vice versa) in US vs EU.
Read the nuance they are concerned about - these are head and neck experts from across the country at major institutions wondering if the 5% dose differences matter - subtle prescription changes / subtle fractionation changes perhaps impacting outcomes.
In breast after all, we’re able to demonstrate toxicity differences within what we believe to be 1 Gy - 27 vs 26 Gy - a bit less than 4% dose and we believe we measured real toxicity differences (FAST-FORWARD ref). As we improve our knowledge, we continue to refine our answers.
And I’ve argued for a while that as we move towards hypofractionation or ultrahypofractionation or SBRT, the edge between good results and toxicity events becomes sharper - ie there is less and less room for error.
SUMMARY:
It is within that context that I think the answer today is quite clear. It is more clear today than in the past because of new information. And I believe on a broader scope, it is more critical today than ever before in light our recent history, where very strong health policies were enacted with a sparsity or even complete lack of randomized evidence. As scientists, we must ensure standards.
To me, the uncertainty that we acknowledge paired with our enhanced understanding of toxicity forces one answer:
Randomized data are absolutely required.
And as we have reviewed previously, data is now forthcoming. It sets the table for an interesting period for our specialty - either way - better or no better - the landscape will be affected.
We Require Randomized Pillars
If you think of proton data as a building or a table upon which a segment of our industry will be built upon, there are clearly some regions where obtaining randomized data will be difficult to impossible. Take for example an integral dose argument in a pediatric patient. Late toxicity differences or second malignancy differences might take decades to appreciate. If the role of protons for the next decade is to assist in the most difficult and unique circumstances, then inherently randomized data will often be lacking.
But we can not rely upon retrospective data or even “prospective” registry studies out of the US market. Proton centers have struggled for viability - many going through “restructuring” or all out bankruptcy. If you believe that during those times that the priority is to maintain the registry database, I can just tell you - it is not. Those are places you cut to the bone, not items that are supported. Yes it is fine to do work in those databases, but the data is not strong. Not near to the level that our industry must be built upon.
So when you read the title of this article, do not think that we require randomized data for every setting, but we do required a number (say a handful) of really strong randomized trials to clearly demonstrate benefit at least in toxicity reduction across a number of sites that create pillars on which we can build the argument for more broad use. And today, 30 years in, that is lacking.
We Sit at the Crossroads
There are two primary options - current studies demonstrate benefit or they do not. Finally, a number of trials will have data forthcoming quite soon.
If they do not show benefit, then I believe the industry must really pause and consider the scale and scope of investment. If well designed trials in head and neck cancer, high risk breast, esophageal, lung and brain are equivalent, then we now must begin to aggressively parse even the highest benefit cohorts of those subsets. A far cry from the promise of protons that is advertised.
But if trials land like the esophageal data and do demonstrate benefit in toxicity reduction - say with head and neck studies both in the US and Europe landing in favor of protons, then we have a different issue. Overnight, we will have real issues with lack of access to treatment demonstrated to be beneficial. Even one trial in a broad patient cohort immediately results in far too little access.
To me, we need to be having that real conversation on a national level today in my assessment to address this issue - a positive proton result is 10x the scale of negative trials in complexity and ethical difficulties. Planning and changes of treatment and referral patterns generally take time. The shocking shift to shorter fractionation overnight during covid was the exception. After all, here we are today discussing a quote from 1999 and in ways, we are today where we were then.
So yes, randomized data is required, but we need to prepare for both results from those trials so that we can quickly adapt in an ethical, thoughtful, and balanced approach.
(As always, the opinion of one. Comment below if you think I’m off target.)
In a few weeks, I plan to return to this topic with some predictions on how we might adapt in light of a positive result in head and neck cancer - to me the most likely scenario in the most likely group of patients. It indeed is an interesting time to be pushing for better. Thanks for following along.
REFERENCES:
Relative biological effectiveness in proton beam therapy – Current knowledge and future challenges





Brilliant summary. Proton$ must exist because the money has been spent to build it. There is so much sloshing around that a company that helps Proton Centers get paid (for a %) cleared many millions in income. Tell me it's not about the money and you have found the person who is getting paid. IT'S ALWAYS ABOUT THE MONEY.