Prostate Cancer: A Tale of 20 yrs: Standards...
It is time that we come full circle - back to greater focus on outcomes.
In my last article, Part 3 of my SBRT Prostate Journey, I finished arguing that we should be more reliant on PSA kinetics. I was running out of room and needed a bit more space for discussion. In that article, I finished with these statements regarding the benefits of a kinetics based approach.
Why kinetics?
Because kinetics minimize effects of early reporting of long-term results.
When comparing cohorts, kinetics minimize effects related to disregarding clinical outcomes. (ie bRFS vs RFS)
Kinetics minimize the impact of when PSMA scans are performed.
Kinetics can be more simply reported at earlier 1 yr and 2 yr timepoints.
Kinetics don’t fix everything, but I think they move our reporting in the correct direction - away from potential bias. At least, from my perspective.
20 years and we’ve come full circle:
I was blessed to train during a time in our field when 100% of our effort - or close to it - was focused on increasing to maximal tolerated doses to increase the cure rate of prostate cancer using radiation. It was a spike in activity and research that set the table for the next 20 years of work we have performed since then.
In my prior post, we discussed that over time, we have (my opinion) slipped a bit in some standards - primarily with respect to median follow-up time vs. reported outcome times. And secondly in a more broad move to report biochemical disease free survival separate from progression free survival. Each of these INDIVIDUALLY often represents an upward bias in our reporting of results of 5% or more.
In a way, I think you see that our field needs to come full circle and use kinetics to refocus on outcomes. I’ll try to explain.
I think back some 20 years to when the Phoenix definition was rolled out. I remember back then not loving the shift to Phoenix definition. I thought it was too easy and maybe (at least in part?) implemented to make our results simply look a bit better. That was my impression - that we moved in that direction as a way to help us compare more favorably to surgical outcomes at that moment in history. And there is plenty of older published data that does tend to show an “improvement” of about 5% with the change to Phoenix from the older ASTRO definition - here is a 2008 reference out of Fox Chase as an example (ref 1).
Granted, Phoenix is has been very robust in the last 20 yrs and it is a credit to those original writers of that definition. But it did “artificially” move outcomes higher almost instantaneously.
Fast forward to today and I think we are likely just better than surgery. Head to head, I think radiation offers less toxicity and very likely, better single modality cure rates - we are consistently moving towards 90%+ control in disease up to unfavorable intermediate risk disease - with NO ADT - if and when we emphasize dose.
PACE A: Randomized Prospective Comparison
Surgery vs. Radiation Toxicity
Look at the recent PACE A presentation of toxicity data (ref 2). Urinary incontinence was 47% (Surgery) vs. 4.5% (Radiation - SBRT) - a massive 10x difference in the number of men requiring a pad / diaper at 2 years.
Read that again. 47% vs. 4.5% - at two years, with surgery 1 in 2 wear a diaper/pad and with SBRT radiation 1 in 20 wear a diaper/pad.
Further radiation wins again on a large scale for EPIC sexual subdomain scores as shown below:
Below are EPIC SHIM (Sexual function) Scores - Higher is better - zero is zero. Surgery falls rapidly and never comes close to recovering even towards radiation outcomes.
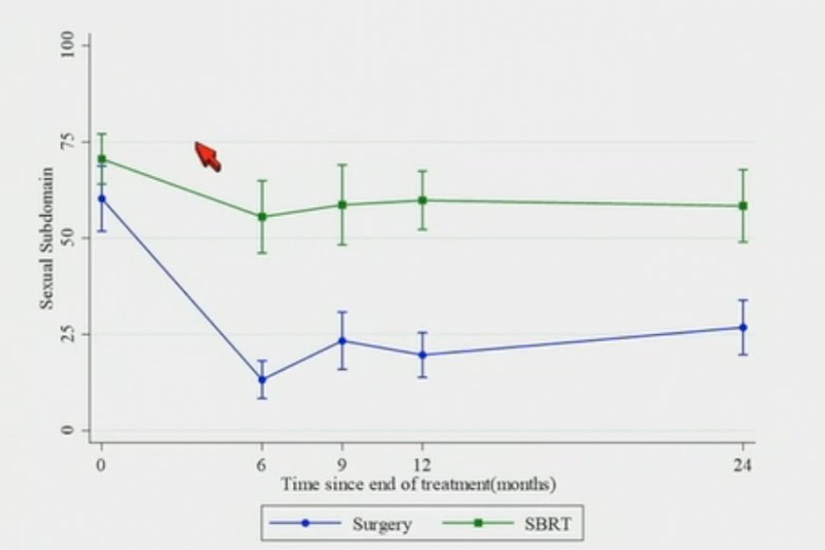
This is data from a randomized prospective trial - likely the best data we will ever have on this topic - this is not internet “opinion”.
Radiation does cause more bowel bother on quality of life surveys - 97.3 for surgery vs. 88.7 on EPIC Bowel bother subdomains. But realistically, bowel toxicity is mild regardless. There were ZERO Gr2 or higher toxicities in either surgery or SBRT radiation arms (a grade 2 toxicity would generally be a procedure like a hemorrhoid procedure - there were ZERO such events / procedures in the study).
But bowel toxicity using SBRT clearly does show up in the patient reported data to some degree - one patient for example in the SBRT reported it as a moderate problem vs zero in the surgical arm. I’ve argued previously when we discussed the COMPARRE Trial that even that difference probably fades away with more fractions (fewer fractions generally means worse toxicity - so if you worry about bowel toxicity, extend the number of fractions a bit more).
My summary: there is some subtle change where SBRT is worse for bowel toxicity but compared to diaper / pad use and massive win in retaining sexual function, it really isn’t close from a toxicity standpoint.
And what about outcomes? They are pending. I do think, in contrast to radiation results back in the late 90’s or around 2000, radiation is simply a more effective treatment for the 5-7 yr cure rate of the primary cancer while limiting salvage treatment across intermediate risk disease but we will see. This PACE A trial will be an excellent resource. My guess is I don’t think we’ll be worse (even with a quite modest radiation dose that appears inferior to higher BED approaches). And salvage rates (for example, radiation after prostate surgery) will be significantly higher on the surgery arm which is not insignificant. After all, if you need both surgery and then radiation - you will see toxicity/costs/time from both.
So back in the day, I think we slightly loosened our standards with the shift to the Phoenix definition for failure. In the following 20 years, I think we’ve further loosened our standards allowing more and more publication of shorter term follow-up series and then amplified that further by excluding clinical failures in some of our highly cited literature. (Discussed in Part 3)
As I’ve discussed at length previously in the “Can We De-escalate better”, we are allowing lower EDQ2 doses to be literally prioritized over higher dose schedules on the basis of convenience and costs - even while data clearly demonstrates more dose cures more intermediate risk disease. In this Substack collection, I have tried to strongly argue this is a poor precedent and bad for our subspecialty.
And today, these shifts carry significant but different risks - not with regards to competition from “surgery” as much as in “alternatives to surgery”. Beyond my concerns for our field with 5% dose reductions or using more ADT or over emphasis on duration of treatment, in the broader view - urology is a terribly competitive space. Other options like cryotherapy or HIFU, to me, capitalize on our softening of standards to enter the current treatment landscape.
A Brief Word on HIFU and CRYO:
HIFU - a recent study 29 patients with 23 months of follow-up showed a failure free survival of 62%. (ref 3)
Cryo - 2021 study with 72 men and much longer follow up of 74 months showed 52% were free of disease. (ref 4) A second study published Feb 2023 using partial gland cryotherapy showed 35% biopsy positive at 18 months with a post treatment nadir of 2.5 (more difficult to assess due to partial gland approach). (ref 5)
My impression: Not on me. Less than impressed. And these were published… I worry what might lie under the rug.
But to their credit, urologists are crafty and this is a “massive US healthcare market opportunity” and one where every prostate cancer patient sees a urologists and then some of them see a radiation oncologist.
And today, there is a new version of hifu - TULSA. It is quickly gaining momentum in some markets and I think is serves as an excellent example of why radiation oncology should continue to focus on prioritizing outcomes - curing the cancer / minimizing toxicity. Once those are optimized, we can ratchet down the number of visits, but if you’ve read much on this Substack, you know that I’ve encouraged us to really work on establishing the highest quality standards. To me, that will serve us the best in the long term.
Today’s “Prostatectomy Alternative”: TULSA-Pro.
I’m in Oklahoma and I thought this was originally just some treatment out of the city of Tulsa or perhaps a Sly Stallone business venture, but neither of those are correct. Here is the explanation directly from the website:
TULSA-Pro for Prostate Cancer
The Transurethral Ultrasound Ablation (TULSA) Procedure is a minimally invasive procedure that uses directional ultrasound to produce very high temperatures to ablate (destroy) targeted prostate tissue. There are no incisions or radiation.
The procedure is performed in a Magnetic Resonance Imaging (MRI) suite and uses the TULSA-PRO® system to ablate prostate tissue from the ‘inside-out’. The procedure combines real-time MRI with robotically-driven, directional thermal ultrasound to deliver predictable, physician-prescribed ablation of whole gland or partial prostate tissue.
My simple summary it is a new version of ultrasound ablation - better technology with MRI integration giving far better feedback on the procedure. And it is supported by and advertised quite robustly by large institutions like: UT Southwestern, Sunnybrook in Toronto, and the University of Oklahoma just down the road a bit from my office.
As a cancer doctor looking at the prostate cancer landscape, I think I’m old and at times think we should just stick to what we know works. But at the same moment, I do love technology and understand the need for progress. On trial with good consents, I don’t think this is an unreasonable path. But even today - this procedure is far beyond that. Show me at least 100 or 200 men with 5 year results before I would consider allowing a family member or friend along this type of path. FDA approval? Yes it has that but please - it was approved on the basis of cutting the PSA in half - heck finasteride does that. (What has happened to our regulatory environment - maybe a topic for some other day)
But to their credit, they are building up data.
Here is data presented at EAU23 in Milan Itay - the TACT Pivotal trial - 115 men treated at 13 institutions, 5 countries. I think this will be updated in a US meeting within the next few weeks. (ref 6)
The goal of this study was whole gland ablation. Tumors were Gr1 and Gr2, <T2b and PSA <15 - so clearly up into intermediate risk disease. Average PSA pre-treatment was 6.3 which is more favorable than a more generic intermediate risk cohort (I’d estimate a broader “intermediate risk cohort” would have a mean PSA closer to 8).
Median nadir post ablation was 0.28 reached at 3 months (this is a pretty darn low nadir).
Per presentation, “PSA was stable between 1-4 years after TULSA”.
I’m less certain about that statement - in fact, I think I disagree (technically they appear to be arguing this based on confidence intervals - blah, “when math fibs” is my assessment). Look above at the graph from the presentation At 4 years 76 men were available and PSA was up to 0.86. From 3 months forward, it appears that the median nadir increased pretty consistently. Salvage treatment was required in 18/115 patients (with 92 and 85 followed for 2 or 3 years respectively - so at 2 and 3 yrs the crude salvage rate might about 19.5% and 21% (I couldn’t find data on when the salvage events occurred or if PSA data becomes censored - minimum crude rate of 15.6%).
Median follow-up is more than 4 years so per Phoenix standards these are 2-3 year results demonstrating that median nadir is still well less than 1 and probably around 0.5 - again this a strong absolute nadir at 2 yrs. 80% have 2 yr data so that still can move some, but likely not a lot. The range of nadirs even at 4 years is still quite low and a median PSA at the 2 yr mark of <0.5 is consistent with nadirs we see within lower EQD2 dose modern radiation series - it is unwise to dismiss this approach.
On the plus side, this appears to be far superior to cryo and hifu reported results. And I say that based on kinetics. See, kinetics are your first early predictor of long-term outcomes - they are the only method to gain longer term outcome insights at I can see.
On the worrisome side to me is the salvage in ~20% of patients and the rising pattern of the PSA beyond 3 months that, at least on this image, appears to show a pretty consistent rising median PSA pattern indicating a higher risk of recurrence with time.
Note: see the CAPTAIN trial below - I do NOT have clarity on whether this trial counts 1 repeat procedure as salvage or not. If you know the answer, please comment. So that could make the “true” salvage rate potentially much higher.
~5% did not reach a nadir of 25% of their pre-treatment PSA and 20% had positive biopsies.
For comparison, my 7250 / 29 series has ~130 patients with a median follow-up of 16 months - to date, one patient has had something done beyond just PSAs and I think he’ll likely will require salvage treatment. That number will increase with more follow-up but we have 40 men beyond 2 yrs and 60 beyond 18 months. (so expected based on this data would be about 8 salvage events). Radiation today is an amazing treatment modality and if judged strictly by curing disease at 7 yrs, I believe quite firmly, today’s high EQD2 approaches would easily win against surgery or these other “surgical alternative” treatments.
More Data Upcoming: The CAPTAIN Trial
CAPTAIN Trial (ref 7) is on the horizon for this new modality - again, they are building data for this approach in a reasonable way - I think this trial has rather large flaws, but this is much better than retrospective analysis or small prospective series, so that deserves kudos.
This trial looks to compare surgery to TULSA treatment. Seems like the trial is for urologists, by urologists - just look at the intro line:
The typical standard of care for patients with localized, intermediate risk prostate cancer is radical prostatectomy, which involves the surgical removal of the prostate.
And no, other treatment options aren’t mentioned.
Trial looks to enroll 201 participants - started enrollment in December of 2021
Primary Outcome Measures :
Safety (12 months) - Urinary Continence - pad free. Erectile potency - erection firmness sufficient for penetration.
Efficacy (36 months) proportion of patients free from treatment failure. Treatment failure is defined as delivery of any additional intervention for prostate cancer (local or systemic, including adjuvant therapy), or metastatic disease, or prostate cancer-specific death.
Secondary Outcome Measures :
Biochemical failure: Biochemical failure is defined as PSA≥ 2 ng/mL for the RP arm or PSA nadir plus 2 ng/mL for the TULSA arm (adopted from Phoenix criteria).
Salvage-free survival: No salvage treatments EXCEPT 1 repeat TULSA does not count as salvage.
There are actually 18 different secondary endpoints but I think you’ve seen enough to get a good flavor for the trial structure.
As you can see above, the Tulsa procedure will use what is essentially the Phoenix definition for biochemical failure - nadir + 2ng/ml. Note that in the surgery arm, failure is defined as a PSA > 2ng/ml.
Does that mean they are withholding salvage treatment in the prostatectomy arm until a PSA of 2 following prostatectomy?? (like I said, a trial by urologists for urologists - I don’t know how that passes an IRB review if they are truly waiting that long - salvage radiation is a known beneficial procedure).
The TULSA arm uses a “Phoenix type” definition - reported at 3 yrs. It will be interesting for me to follow this trial as my patient cohort should have comparable follow-up duration than this study, so I’ll be able to give good comparative numbers for additional local procedures following “whole gland treatment” vs. radiation in a rather live comparative approach.
STANDARDS:
This is why I like clear and very strong standards - eventually softening and opting for “good enough” but “shorter / cheaper” I believe will come home to roost. The PSA kinetics for this new approach demonstrate pretty low nadirs. Based on nadirs, I believe this is by far the best alternate treatment approach (beyond surgery or radiation) to date. And if this data is replicated and holds up, this will be competitive in the marketplace and we’ll have to deal with.
Look at the Profound Medical press release (maker of the TULSA - Pro device) - they do what I would do - they quote a meta-analysis of radiation biopsy positive rate of 32% for radiation making the argument that their 20% is quite reasonable (ref 8). I dug through the referenced radiation meta-analysis so you don’t have to. Here are my quick points:
seldom high dose modern radiation - greater than 1/3 of studies used a four field box approach as just a simple example.
if you followed NCCN the biopsy positive rate fell to 22%
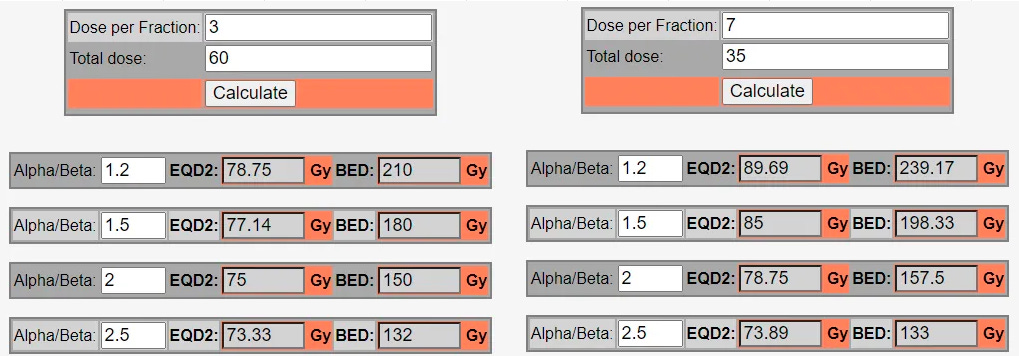
Zelefsky has two of the series in SBRT series (ref 9, 10) and his work shows the importance of dose:
Dose / fx = positive biopsy rate
32.5/5 = 47.6%
35/5 = 19.25%
37.5 = 16.7%
40 = 7.7%
But what do we do?? Well, NCCN offers 60/20 fractions as “Preferred” for intermediate and high risk cancer, but oops - that is less dose than 35/5 where 20% of people still have biopsy proven disease. But in higher dose series, our positive post-treatment biopsy rates drop to around 10%.
This basically makes my argument for one of my central themes in this Substack - we need to focus on excellence in outcomes. So when we lower our expectations and standards, it definitely trickles back into arguments against our approaches. And have no misunderstandings, you can’t argue “good enough” 364 days a year and expect anyone to listen to your stance when you change gears on day 365.
And if you publish data that ignores clinical failures and you focus only on biochemical relapse free survival, I believe you really can’t effectively argue against repeating the TULSA procedure as a salvage procedure - after all, you ignored clinical bone metastatic disease. Again, a slipping of standards has consequences.
So TULSA really is a good example of: 1) why we must focus on superior cancer outcomes and 2) illustrating my rationale for emphasizing kinetics.
Above in the TACT Pivotal trial, I believe kinetics show us that the directional trend is wrong. In radiation series, the median PSA decreases with increasing time - you see more failures with longer follow-up but the median nadir (not MEAN, median) just tends to go lower and lower.
For example, in the Consortium Ma publication (ref 11 ), median PSA at two years is 0.33 and falls to 0.18 at 6 yrs. Or take the much older Cleveland Clinic data (ref 12) treated from 1987 - 2000. It has quite low doses of ~70 Gy, and even there, the trend is lower with longer times.
Summary of Table 1 demonstrating lower PSA nadirs with time:
839 total patients in the study reports numbers reaching a specified nadir:0.5 ng/ml - 12 mos: 121 pts, 24 mos: 287 pts, Any time: 412 pts
0.2 ng/ml - 12 mos: 36 pts, 24 mos: 98 pts, Any time: 211 pts
With time, more and more patients hit nadirs of 0.5 and 0.2. Looking at the data, the entire series nadirs around a median of 0.5 - higher than Ma (makes sense as these patients got less dose), but still good enough to have lower median nadir with more and more years.
So even at 70 Gy - dose that is clearly insufficient in intermediate risk - nadirs continue to fall and we know long term control at 70 Gy is ~78% at 5 yrs falling to 59% at 8 yrs from the MD Anderson randomized data (ref 13). And at around 80% control, you start seeing clinical outcomes differences in those reaching low nadirs vs. those that never get that low. So if we don’t hit 80% disease free survival at 5 yrs those men have higher metastatic rates and higher prostate cancer mortality (think back to the old dose escalation Memorial Sloan Kettering data 2yr 1.5 nadir data as a second example - ref 14).
And yet, here with TULSA, these patterns are clearly different and I think it will ultimately lead to worse cancer outcomes than a 70 Gy radiation approach - so worse than 59% at 8 yrs disease free survival. My guess is the range is smaller than anticipated due to an increased use of salvage in the TULSA setting that blurs and affects the failure rate / kinetics, but time will tell whether this is correct.
There is a chance that radiation vs. other ablative approaches have drastically different kinetics, but I doubt that is the case - my guess is ablative is ablative. Look at the trial design - they used an adopted “Phoenix definition” - they think it is similar and so do I. And based on our history of outcomes during dose escalation, depending upon how these series mature and complications from salvage (which is currently marketed as safe with really no data that I can find) , these deviations from current standard of care have real potential to cause real clinical impact due to increased risk of metastatic disease and prostate cancer mortality if 5 year outcomes are less than 80% - especially when compared to the best of the best - ie high dose radiation approaches.
Quickly return to the rising MEDIAN PSA nadir: In TACT Pivotal trial, at 3 months - 50% have a PSA less than 0.28. If 51% simply stay less than 0.28 - the median will not move. That is what we see in radiation series - over half are cured long term using doses down to 70 Gy and the median continues to fall - at least through ~4 years. Here, in rather stark contrast, at 4 yrs half are above 0.86 and it appears from the graph that lower bound of one standard deviation is ~0.28 meaning ~16% have true “stability” of their PSA nadir (std dev includes 68% - half of 32 is 16). Quite different and in part why I’m confident radiation is far stronger curative approach.
And this is why I like kinetics: When you see results published for the TULSA procedure, I believe the only way to compare the results to our historical data will be PSA kinetics and how many patients required salvage treatments. Those two factors will tell us far more, at an earlier time period, than the Phoenix definition. If you agree, then you like kinetics as well.
(Hint: if you have a voice on our national scene, help us to publish more PSA kinetic outcomes - or comment and convince me otherwise).
And in our own radiation literature where we have standardized “any dose” using “any fractionation” (my exaggeration of our guidelines), kinetics can do the same thing to help select the very best cancer curing approach from those that are inferior. The more we accept that shorter is just as important as optimizing the cancer treatment outcome, the less ground we have to argue against surgeons doing quick, convenient, multiply repeatable, expensive procedures.
Two final parting thoughts:
The TULSA procedure will put more pressure on our specialty because it appears to have an opportunity to be a different path that approximates our outcomes with lower EQD2 approaches that some (not me, but NCCN) recommend as standard of care. Moving forward, we need to AT LEAST either 1) prove superior cancer control or 2) shorten our approaches to offer SBRT more broadly. I still believe we are relying to much on the later approach and not enough on the former.
Much of our current history and rationale for prostate cancer was built on treatment of low risk disease. The days of mass treatment of low risk disease are over - many of those rules / themes no longer apply. With higher risk, disease failures have greater consequences. And with technology improvements, we can safely dose escalate while limiting toxicity often leaving recurrence of the cancer as by far the worst treatment outcome. Like the title says, in ways it has been a 20 year journey and we need to come full circle. It’s time to refocus on optimizing excellence in outcomes and continue to prove our top tier results are superior.
REFERENCES:
The Phoenix definition of biochemical failure predicts for overall survival in patients with prostate cancer
https://pubmed.ncbi.nlm.nih.gov/17968996/PACE - A: Toxicity comparison of surgery vs. SBRT
https://www.urotoday.com/conference-highlights/asco-gu-2023/asco-gu-2023-prostate-cancer/142476-asco-gu-2023-pace-a-an-international-phase-3-randomised-controlled-trial-rct-comparing-stereotactic-body-radiotherapy-sbrt-to-surgery-for-localised-prostate-cancer-lpca-primary-endpoint-analysis.htmlSingle-center, prospective phase 2 trial of high-intensity focused ultrasound (HIFU) in patients with unilateral localized prostate cancer: good functional results but oncologically not as safe as expected
https://link.springer.com/article/10.1007/s00345-023-04352-9Prospective trial of regional (hockey-stick) prostate cryoablation: oncologic and quality of life outcomes
https://pubmed.ncbi.nlm.nih.gov/33454813/Cryotherapy for partial gland ablation of prostate cancer: Oncologic and safety outcomes
https://doi.org/10.1002/cam4.5692Profound TACT Data Press Release
https://www.globenewswire.com/news-release/2019/04/04/1797449/0/en/Profound-Medical-Announces-Positive-Topline-Results-from-TACT-Pivotal-Clinical-Trial-of-TULSA-PRO-in-Patients-with-Prostate-Cancer.htmlA Comparison of TULSA Procedure vs. Radical Prostatectomy in Participants With Localized Prostate Cancer (CAPTAIN)
https://clinicaltrials.gov/ct2/show/NCT05027477Long-term biopsy outcomes in prostate cancer patients treated with external beam radiotherapy: a systematic review and meta-analysis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8384630/Five-Year Outcomes of a Phase 1 Dose-Escalation Study Using Stereotactic Body Radiosurgery for Patients With Low-Risk and Intermediate-Risk Prostate Cancer
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7525798/Early Tolerance and Tumor Control Outcomes with High-dose Ultrahypofractionated Radiation Therapy for Prostate Cancer
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7402022/Refining the definition of biochemical failure in the era of stereotactic body radiation therapy for prostate cancer: The Phoenix definition and beyond
https://www.thegreenjournal.com/article/S0167-8140(21)08797-1/fulltextEarly prostate-specific antigen (PSA) kinetics following prostate carcinoma radiotherapy: prognostic value of a time-and-PSA threshold model - Cleveland Clinic data
https://pubmed.ncbi.nlm.nih.gov/15221994/Long-term results of the M. D. Anderson randomized dose-escalation trial for prostate cancer
https://www.redjournal.org/article/S0360-3016(07)01173-X/fulltextPostradiotherapy 2-Year Prostate-Specific Antigen Nadir as a Predictor of Long-Term Prostate Cancer Mortality - MSKCC
https://www.redjournal.org/article/S0360-3016(09)00045-5/fulltext






Great post, though one quibble I have is of 60Gy/20fx being not “high dose.” The PROFIT trial showed equal biochemical control with modern, dose-escalated conventional frac.