Proton Therapy: "Study of the Year" Edition
A look back at 2023 from a proton therapy perspective
As the year end lies on the horizon, we’ll take a moment and look back at some of the more influential proton therapy articles. And if, I’m being honest, it was far less exciting than the progress in SBRT.
I mean, there was this journal cover on a proton oriented publication for an article that basically says - if you use standardized blocks and do not have a custom compensator, one can get the costs for protons down to about the cost of photons. But is that really where we are? Using protons to create quite poor dose distributions? Is it really that bad…
Well… maybe…
$50 million Proton International Center at UAB closing over ‘inability to make payments’
This was just announced November 28th. Not restructuring, closing.
In a statement, a UAB spokesperson said the center will close due to center partner Proton International’s “inability to make payments to bondholders, equipment finance companies and other vendors.”
“While UAB will continue to offer extensive treatment options for cancer patients, we are working with Proton International of Alabama – as manager of Proton International at UAB – to wind down operations and close the proton center,” the statement reads.
Yikes. It opened just back in January 2020.
I literally lasted longer in protons than UAB.
But, if you just back up and look at my Substack, we know this type of debt level can’t fly. Back in June I wrote that, generously, one gantry can support $20M-$25M - with great contracts and patient mix - maybe $30M. With any bloat in the system, the number is likely closer to $15M if you don’t have crazy good insurance payment rates - well beyond the 2-4x Medicare rates that most will see. It’s just basic, back of the envelope, math.
I wrote this article now 6 months ago on the money side of the business.
Protons 101: That Money / Cost Thing
It begins….
To say that protons are controversial is a vast understatement:
“Proton-beam therapy is like the death star of American medical technology; nothing so big and complicated has ever been confronted by the system,” said Amitabh Chandra, a health economist at Harvard University’s John F. Kennedy School of Government. “It’s a metaphor for all the problems we have in American medicine.”
But it goes on to put costs in perspective and explain how I arrived at those figures and what the bond market looks like on a broader scale.
Here at the facility on the UAB campus, the debt was nearly $90M (Ref plus there is about 8M additional debt via the vendor - so the reality is far more debt than the news headline number of $50M).
Regardless, there is simply no way it was viable without charitable support, or the institution picking up tab, or a formal restructuring of the debt. Those are the three options that keep the doors open and I guess, the forth is closure. Bondholders best be prepared for literal pennies on the dollar. FYI: I think it’s likely to reopen in the future as a truly owned / operated UAB facility - at least that is my guess - we shall see.
Wait, there was this bit of positive news:
When insurers turned down patient’s request for cancer treatment, they didn’t know he was a top trial lawyer
Is that positive? It was reported like it was - kind of. And it is a story about “the little guy” (kind of - I mean he has access to a private jet) fighting against insurance authorization - a place where, I do think often “insurance companies” act as “physicians” making clear medical decisions - but I digress. And it is for treatment of a head and neck cancer - a treatment site where I think there will be randomized prospectively proven benefit at some point in the near future (we’ll see).
So maybe it is a win. I think on some real level, it is a win for clinicians and patients fighting for autonomy in our healthcare system - that part, I’m pretty sure about. A true win for protons? I’m far less clear about.
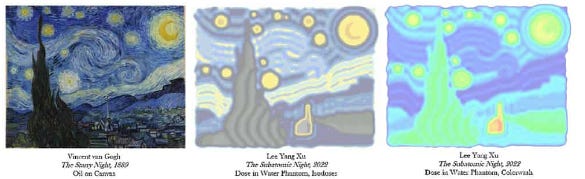
Oh!! And we can use $20M+ machines to create artwork using protons!!
But seriously…
No wait… I have one more…
We’ve all heard about the great strides that AI will bring to our field - surpassing the talents of many in so little time. So, I asked Grok to write me up a spicy proton ad. And it gave me this - first attempt - blow it up, read it, well-worth the read:
“wilted flower in a field of healthy ones?” “Superhero of cancer treatments”. Leaving healthy tissue “feeling like it just had a spa day”. “No more side effects that make you question your life choices.” “1-800-PROTON-POWER.”
I stand corrected. AI has already surpassed every marketing team ad I’ve ever seen.
I jest - kind of…
All kidding aside, you are on a “proton” site with a physician who actually likes protons and still believes that they do play an important role in the future of radiation. I picked up my life and practice in a search to find better. I did so, primarily for head and neck cancer - still a place where I believe it delivers benefit. And I still think - that over the next few years, we’ll see far more wins than the existing Esophageal data. Time will tell. But for 2023 - a year of pretty great progress in our field, we have rather limited candidates for the proton trial of the year.
There were some minor claimed wins - LET work, FLASH work, heart dosimetry work, and nasopharynx work etc - but little really demonstrating protons > photons in a clinical setting. Looking back I leave the year largely with the same proton therapy front-runners for adult cancers related to their long-term positive impact (well, we might add one):
Esophageal prospective trial
Bauman Concurrent retrospective comparative trial
A large collection of Head and Neck data
I’m still looking for the “promise of protons” trial. Here is my language from 2019 on this describing the goal of proton therapy:
To me, the “promise of protons” is in the Bragg peak and in the dosimetry slides. Protons provide less dose to normal tissues and therefore must end with less toxicity across a broad spectrum of disease sites. It is the center of the marketing campaigns for these facilities. That is the bar that has been self-set by this industry and one that needs to be cleared.
And that is what I’m looking for. Not cherry picked sites or highly selected sub-cohort populations, but rather significant and broad impact on par with the required additional capital outlay - consistent with the difference you can see on the plans - that is the actual promise that the proton industry has made. This is the bar that needs to be cleared with prospective, randomized, high quality data.
Here are my top five candidates for the broadest positive impact studies for the year regarding proton therapy:
5) Lancet Oncology breast article
Protons can hypofractionate in breast cases.
When a trial lands in Lancet Oncology, I think it should be considered. Ironically, this can be viewed negatively or positively, but as a clinician practicing in a proton facility with only about 5 years experience in this area, I was pleased to see the data supporting what we have been doing in OKC for the last few years. In OKC, after year 1, we’ve been moving more and more patients towards 15 or 16 fraction approaches - I personally picked the 4005 cGy over the 4256 cGy because it is cooler and therefore, I thought it added one “fraction” of safety should there be any differences. That program continues to grow and we essentially now fractionate how I would with photons. This substantiates that effort.
Clearly, you can argue that protons should have done this work, and published it back by at least 2013. I think that is a reasonable position, but for the year, this is one of papers demonstrating progress in the proton literature - for better or worse.
4) Head and Neck Japan Data
This was published recently out of Japan and it adds to the large segment of retrospective data showing that protons appear to have less toxicity in the treatment of head and neck cancer. Based on the volume of data and now, 4.5 years of clinical experience, I think this is real. I think this will be proven at some point in prospective data. I’m hopeful that data will begin to come out in 2024, but we shall see.
Here the study showed improvements in all-cause mortality, cancer-specific death, and local regional recurrence. Proton therapy for local regional recurrence showed a hazard rate of 0.61 for example.
But ultimately, it is retrospective and from a proton perspective, the clock is ticking. At the same time randomized data is accumulating, we are moving towards significant options for de-escalation of nodal dose and targets more broadly in the photon world. Successful de-escalation will make the opportunity for improvement less and less - harder and harder to demonstrate a difference.
3) MDACC Prostate study
Covered on this site here:
Headlines were these two numbers: UIR 94.3% (82.1% ADT), HR 86.1% (100% ADT)
By any standards, those are high marks. Proton therapy achieved pretty darn high disease free survival - especially in UIR and HR cohorts. This was 7 year median follow-up and appropriate 5 year results - but it is retrospective.
At release, I actually thought the results were quite strong - one of the front runners for the year. But once the randomized controlled trial on the photon side came out (PACE B), it seems far less impressive. Basically both datasets significantly outperform older data. So once the randomized data did the same, it clearly becomes less impressive and the fact it is retrospective is a clear second detractor.
I predicted back earlier in the year that the proton prostate randomized trial would be negative. Paired along PACE-B, I’m going to stay put.
2) Lung - Lymphopenia risk article
At a close number two on the list, we finally get to a study that has far less issues. This study shows that protons reduce lymphopenia risk - based on a prospectively collected series of consecutive patients with stage III non-small cell lung cancer. It used modeling to predict benefit and then treated that select cohort with protons.
271 (200 IMRT, IMPT 71) patients were enrolled - median age of 66. The incidence of Gr3 lymphopenia was 67% (IMRT) vs. 47% (IMPT). Anemia risk was 26% vs. 9%. About 10% fewer patients in the IMPT arm declined from a PS standpoint and 20% more patients in the IMPT arm were able to receive standard of care durvalumab (74% vs. 52%).
This appears to be quite strong data and I like that it is prospective and consecutive and used selection criteria to stratify patients. It looks at pencil beam scanning and demonstrates a win that is consistent with the literature more broadly - less hematologic issues for patients receiving concurrent chemotherapy and radiation for advanced lung cancers. Yes, the old MD Anderson passive scanning lung trial was negative, but I think we still learn a lot from negative trials and it pushed us in the chest to learn and push a bit harder.
It’s strong data. Clearly selection bias is a real possibility but it an article that I’ll come back to in the future as I need a bit more time to unpack it in combination with this new pneumonitis data. And yes, this is an area in both lung and esophagus where we should have randomized data within the next few years.
And finally…
1) Protons Outperform TACE in a randomized prospective trial
Protons demonstrated in randomized controlled trial that they are superior to TACE - the most commonly utilized procedure for liver cancer. It’s proton data and it’s doses that aren’t used in photons very often. Protons win on local control. Protons keep the patients out of the hospital - eliminating 85% of patient time admitted to the hospital. And protons win decisively on cost.
I wrote it up here and walked through examples of the difference and how and why protons really do make this site far easier to treat.
I think it creates a new standard approach - and I think that standard is proton based for many cases. It demonstrates that protons outperform TACE. Protons can simply give a lot of dose to liver disease with even less impact of the adjacent liver compared to photons which is highlighted in the more thorough discussion above.
To be clear, I think SBRT is clearly superior to TACE for local control as well, but my assessment is - the dose escalation is easier, and lower risk using protons. As I’ve said, you simply get dose escalation almost for “free” within many plans (see article above for examples).
The main obstacle for this study is has is simply that, even within our own field, the majority of radiation oncologists will not quote the data or refer patients to a proton center - even for the tough cases. Instead, they’ll keep them “in-house” and do their “SBRT approach” and rationalize that the dose differences are quite minimal with respect to the final clinical outcomes. To what extent that is correct, I’m less convinced. But here is a fact: since release of this trial, at our proton center, in a busy liver clinical environment, I’m aware of 0 referrals from "beyond our facility” since this publication. Zero.
And that reiterates one of my points:
When data doesn’t fit your business model, it ultimately looks quite similar - whether you are in the proton center arguing for use or whether you are across the street from the proton center arguing against them.
As I’ve written, proton therapy, due to its capital costs and limited access, remains divisive. And current systems make it amazingly unlikely for patients to be sent beyond institutional walls. For many, it’s probably kind of funny to laugh at the failures (or lack of major progress) of the year and, at the same time, more difficult to read and consider the reality that are likely times and places where protons are increasingly likely, just better.
Today the size of the cohort where that benefit is proven is pretty darn small. But for the first time in our history, we have a mountain of randomized data that is building up across the globe with pencil beam approaches. It will be interesting to see where it all lands as it comes sliding down the slopes.
Likely on both sides, there will be pieces to pick up following the avalanche. An interesting time indeed. Next week, we’ll wind down the year looking back at the year here on the Substack and look at the top articles, as chosen by the readers - based on reads.
In the meantime, have a wonderful holiday season. Merry Christmas!!
If you made here and agree, hit the like button - these things really do help. If I messed up, leave a comment. Thanks for following along this year as we search for better. I anticipate next year will be interesting as well.







In 2005 I started using the Cyberknife because of its precision and accuracy. In 2008, I literally walked out of an investors meeting for a proton center because I could not clearly see an advantage for most adult patients. (That facility later went into bankruptcy) I still review the proton data to see how I could improve my dosimetry. For example, I now limit the dose to the left atrium for my esophageal patients to reduce the risk of AF. It is easy to do without increasing the lung dose. (Red J 2024;118:124) Also the ACR guidelines allow for smaller CTVs and PTVs than used in the study. (Red J 2021 Jan1)