Prostate cancer: An SBRT Journey: Part 1: The Backdrop
My journey into SBRT prostate cancer treatment that led to my re-assessment of the literature.
As always, author of one. If you see an error, please reach out or leave a comment.
SBRT: In the US, defined as 5 or fewer treatments - high dose per day, short fast overall course. It has been one of the main drivers of our field over the past two decades - for example, it has had tremendous success in lung cancer, some brain tumors, and metastatic disease dramatically increasing our cancer control rates. Today, we are building up great prospective trial data in prostate cancer, but until that is available, we use the data below.
This Substack is, in part, about my journey to a proton center. Today we’ll talk about my SBRT experience with Uniform Scanning Proton Therapy. In the big picture, this story serves as the backdrop for my closer reassessment of the data and literature. I hope it gives context to my questions / uncertainty regarding what I see in SBRT for prostate.
Protons 101: Prostate Series brief summary to date:
The COMPARRE trial review - an article discussing that I believe it will show no difference as structured - speaks to Phoenix definition at 3yrs and IMRT / SBRT improvements with SIB leaving the opportunity to demonstrate improvement in the past.
Non-Inferiority trial design - This reviews my general dislike of non-inferiority trials which form the basis for most standard of care options for prostate cancer treatment today.
Refocus on Cancer Outcomes - An editorial where I describe that I believe we have moved too far away from a focus on outcomes best outcomes and too often are complacent with “good enough” results.
Can We De-Escalate Better - This is a large scale review of our literature and the data supporting NCCN recommendations - it asks if can we stop using ADT in unfavorable risk disease instead of just trying to drop fractions - I argue yes. We need a high bar for local regional control of at least 90% at 5 years, but in that context, I think the historical data favors avoiding ADT.
PSA Kinetics - 1 yr and 2 yr metrics - A review of data supporting early PSA kinetics that one must meet in order to achieve 90% 5 year DFS in prostate cancer which is critical to achieve IF we are to avoid ADT. Mean PSAs: <1 at 1 yr and <0.5 at 2 yrs.
And today we’ll begin to explore my clinical journey into SBRT for prostate cancer treatment. Up front, I have very limited prostate SBRT experience. I don’t recommend anyone replacing the opinions of leaders in the field with my assessments, but rather consider integrating what we will cover into your perspective of the data and where our field of radiation oncology needs to go. Despite limited SBRT prostate experience, I’m pretty confident in my general prostate knowledge and ability to read literature. Plus I’ll review some of my own personal outcome / kinetic data that now has 220+ patients treated with protons. As always, you decide.
Originally, it was an article, then two. And now a small collection. I like them to be email-able for subscribers so I’ll try to stay within that framework and the pieces became import enough to warrant their own post, so here we go.
My SBRT Journey: The Story
Prior to OKC, I was in North Little Rock and in the last 5 or so years, the dominant urology group owned and operated a machine so my prostate volumes were pretty light. I generally treated to 78 / 39 but was transitioning to 70 / 28 or 60 / 20 but I was treating like 10-20 cases per year - some years less - relatively low volume. In my clinic, I didn’t do SBRT in general - satellite center - limited physics coverage - this was 2017ish and just had stayed simpler.
Over the course of my career, referral patterns shifted back and forth and if you’ve read prior posts, I had a lot of traditional fractionation prostate experience. I did implants back in the day, but not recently. There were busy years when the urology group leased time or prior to their linac ownership, but in the lead up to the move to Oklahoma City, it was quite different and volumes were quite low.
I have no long term history with SBRT for prostate - closest was LDR brachy from back in the days of Seattle (ref 1) and Critz (ref 2) (old references for young people to see history in our field) and in training at MDACC with Pollack starting that program while I was there. Nothing with Cyberknife and really even very limited hypofractionated experience in prostate cancer. I remember shifting to 4256/16 for breast in 2009, but I don’t remember dates for prostate cancer - but mainly 78 / 39. I read some of the prostate literature but cursory level, not deep in the weeds. I was treating with what I had used for 20+ years.
Moving to OKC, I stepped in and basically continued what had been done at that facility. I had no hands-on proton experience. The center was the 6th one in the US opening in 2009. The center represents a large segment of the Proton Therapy Co-Operative Group (PTCOG) uniform scanning data. So at first, I did what the center did - 7920 cGy (RBE) in 44 fractions - long course traditional treatment. I worked alongside Les Yonemoto and ran every case by him for about 3-4 months - he had decades of proton experience (thank you again). John Chang - head of the peds PTCOG section with over a decade of proton experience - showed up in month 2 and away we went. We had big experience in both our physics and dosimetry teams - it was a wonderful opportunity to “drink from a firehose” and learn a ton nearly 20 years into a career.
As I gained experience, I started looking at ways to shorten our approach. Obviously that is where our field is headed in a big global perspective and I thought it was important that we moved in that direction. So probably about 3-4 months in I started looking at 7250 / 29 fractions based on the Florida experience and began enrolling men in an SBRT trial comparing 38 / 5 fractions vs. 7920 / 44 (ref 3). I would say that isn’t the easiest randomization - very much all or seemingly nothing. Especially when the the majority of off trial patients were being considered for something in the middle with 29 fractions.
But that was the path forward. Per the protocol, the only real difference was strictly the fractionation and dose. I believe the trial is completely closed and chart reviews for this study are underway currently. I believe data is expected around December of this year, but not sure on that timeline.
When I arrived, I thought this was the path - an SBRT approach. And SBRT with protons? - maybe that would be better - “youthful enthusiasm” during what many might call a mid-life crisis of sorts moving states and practices. But I enrolled patients on the protocol and off we went.
Shortly thereafter, I started treating a few more men from out of state with SBRT if they wouldn’t consent to the option of 44 fractions. I was asked to join up with Mack Roach as Medical Director of the OKC facility and was one of about 15 physicians worldwide on the initial calls for his push for a large photon, proton, carbon SBRT trial (don’t know where this is today - I stepped down as Medical Director after about 2 yrs in OKC). Regardless, I was on board and actively trying to move in this direction rather quickly.
So the first handful or two were largely on trial then I started expanding to those with lower risk disease from out of state. Off and running so to speak.
And then just as I started to ramp, I thought the toxicity was higher.
I thought clinically both bladder and bowel toxicity acutely were higher and one early patient had toxicity post treatment I didn’t like (purposefully vague as really don’t know if he was on protocol. All sign releases on trials /registry etc, but being careful). I had been at the center for about 1 yr and had seen very little toxicity with 7920 and my “newer” 7250 / 29 approach. This seemed different. I tend to be very cautious and clearly these were small numbers but this was my first mental note.
The SBRT trial was daily treatment and our center always included a weekend, so W,R,F,M,T as an example. Based on the toxicity I thought I was seeing and some of the SBRT data showing we can spread these out to improve toxicity (data supports up to once a week treatments), I moved the off-protocol patients to every other day, then even to 2 per week to cover two weekends for some - I would condense back to three in wk2 if doing well for some if week 1 was uneventful.
Toxicity seemed better with more time and I thought this was the path. But then post-treatment PSAs started rolling in from the very first handful and unlike the 7920 and even 7250 / 29 fraction approaches, they weren’t falling super fast. So I tweaked the dose moving from 38 Gy to 40 Gy for intermediate risk cases (John Chang had used 40 Gy pretty routinely over the prior few years and was using that at the center so I was comfortable). And again, at the time I was on the Roach calls which was looking to expand to UIR disease so I was trying to move up in dose to move towards that setting.
Historically my standard was 78 Gy / 2 Gy per fraction with IMRT. I hadn’t changed since leaving MD Anderson. Patients seemed to respond well - low toxicity, low PSAs. But I did NOT track my prostate data for years and so I really don’t know with certainty how they did.
Would it surprise me if my average nadir was above 1 with IMRT? No. Even 1.5 or 2? Not shocked. When I moved to the proton center I *thought* labs were lower, but so does everyone who moves to a proton center (haha). Realistically I had no idea. But within the first 10-15 or so SBRT cases, I was pretty darn sure the kinetics following SBRT were different from either 7920 or 7250. And even though I had limited time at the center, the center had treated 300+ per year and we follow them at about a 80%-90% clip for 5 years - so I was seeing plenty of historical data. SBRT seemed different.
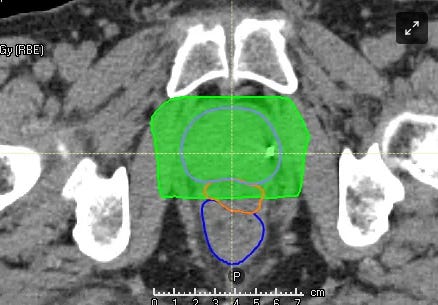
Let me make this clear. I’m obsessive if anything. I fuse my own MRIs every time - if someone else does it - I’ll reload it and tweak it - every time. I contour the prostate, bladder, rectum for every single case I do - always have, always will. There is no person to person variance. I likely hand adjust blocks a mm here, a mm there in 50% of my “routine prostate cases” based on coverage, OARs etc. If there’s a compromise needed, I load it up in my office solo and I tweak blocks, weightings, apps, comps etc - end of the day - its one of my plans. Just pointing out there is no process variable in my work.
At this point, I paused and significantly slowed my SBRT enrollment. I wanted to wait and gather data. Men were travelling for top tier results - not pretty good quick treatments. My stated goal was to produce outcomes in the top 5% of prostate outcomes in the US - maybe arrogant and unattainable as clearly everyone can’t be top 5% - but that was the goal. In my mind, I *thought* with 7250 or 7920 my PSAs were going lower and I *thought* that rectal toxicity was a step less compared to IMRT. Whether that was imagined, or case volume related or due to SpaceOAR or having a dedicated treatment room for prostate or protons or obviously and most likely a combination of factors, I didn’t know.
After all, in moving to SBRT, I *thought* I knew nadirs should be VERY low - like implants. I *thought* I should get to long term results well in the 90s for FIR and even UIR cases. It was more dose. I saw the headlines of great responses and it seemed as if everyone was moving that direction and I therefore set high expectations - you know like 95% DFS at 5 years. But as we discussed, within the initial 10-15 patients, following protocol, something didn’t feel right.
So I opened up Excel and I started my database. Tracking every patient, every fractionation approach in a spreadsheet. One sheet for SBRT, one for 7250, and one for 7920. I needed data. I’ve done this over years for sites like lung and head and neck or new technology like IGRT looking outcomes or toxicity or table shifts as examples - multiple year reviews of my outcomes and practice patterns and it always gives insights.
(I strongly encourage those in training and early out to start this habit. Don’t track more than you can, but in a quick 2-3 yrs, you will know if YOU are replicating the literature you are striving to meet).
And that is where I am today. A slow to paused accrual while I accumulate data. I still anticipate that with long-term follow-up the original low risk men (mostly LR and FIR) will do very well - they should - it was good dose and very low volume / low risk disease.
Initially I wondered if their lower risk and generally younger ages wasn’t the difference in post treatment kinetics. I really assumed that was the case - that it was a patient selection issue driving differences in PSA kinetics post treatment. But now another 15 months down the road treating those same younger / lower risk men with 7250 / 29 and I think it is something more. I have enough similar patients in the other groups to ballpark compare and I still see differences. I’m pretty certain that, at least, in part of what I see MUST be related to the fractionation approach.
A small number of men are on trial so I won’t give any specific data but at year 1 mean PSAs: 7250 cohort is lower than 7920 cohort which is lower than SBRT cohort (very small pt numbers in the SBRT cohort because of what I described above). All three appear clearly different at over ~220 pts total in database some with very short follow-up but all my patients - super low variance in technique as I’ve described. 7250 consistently meets my PSA kinetics criteria for 90% DFS expectations and the others do not (meaning PSA mean for cohort <1 at 1 yr and <0.5 at 2yrs - ie consistent with Ma data we’ll review in the future - for how and why these metrics - read my prior post on PSA kinetics).
Note: 7250 vs 7920 makes sense - EQD2 in 1-2 range is ~74 vs ~82 and the reduction off SVs is at 60 vs 54 so EQD2 of 68 vs 50. 7250 in 29 fractions is a significantly hotter prescription - and as I discussed previously, the volume eliminates a significant margin miss risk in my view.
The EQD2(1.5) for 38 / 5 is even 18% hotter than 7250/29 and 40 /5 is another 10% higher - that is IF EQD2s hold up with simple calcs in SBRT for very low alpha / beta tumors).
Currently I consider the 7250 / 29 my reference dataset. The intermediate risk subset 81 pts patients (~44% UIR), 14 treated with ADT have a yr 1 mean PSA <1 at 0.81. 2 yr data appears to be consistent with a pattern that will be <0.5. It is an immature database and can change, but it is more than anecdotal evidence. I believe these initial kinetics put it on a path to demonstrate 90% or better 5 yr bDFS with this approach with the clear majority of UIR not receiving ADT.
This seems ballpark consistent with the UFPTI data that demonstrates IR control >93% at 5 yrs with very limited ADT use. (ref 4)
In support of SBRT, I do see some slight indication within the 7250 cohort that within the first year post treatment, higher risk disease falls faster. I’ve seen some data showing slower kinetics for normal prostate tissue compared to cancer. I generally do NOT see that in clinical the literature, but few datasets will have as little variance as my series. For 7250, all risk groups are less than 1 at 1 yr (HR and VHR all generally get ADT and are therefore FAR lower) but potentially there is a quicker response with more disease and higher risk disease in the first year following treatment (so UIR falling faster than FIR, faster than LR). But I need more data and more time.
It also should be noted that my experience is in uniform scanning proton therapy making it a rather unique experience. But on the other side of that argument is that it was a multi-institutional trial treatment (or based directly upon) with well defined treatment criteria. As I’ll show later, my experience is not unique and is supported in the literature so while it might be easy to be dismissive of the data due to the proton aspect, I think that is unwise.
So that is my personal context. While I can drop ADT in most UIR and reach a one year nadir far less than 1, that same contour / dosimetry in 5 fractions doesn’t produce that same results in lower risk men - even when doses should be higher. And simply stated, that is why I started to really look at the SBRT data regarding expectations and looking with a critical eye - not just skimming headlines and abstracts.
What else could be going on?
Small numbers - no doubt. You have a small enough sample size and clearly weird things can happen. But just to give a feel for the difference - at 1 yr, the raw number of men in the SBRT subset at 1 yr with a PSA over 2 was more than in the entire 7250 subset that is 9x larger - and my SBRT cohort has the same number over 2 as in the 7920 cohort that is 6.5x larger. It is different.
They are generally younger and significantly lower risk patients. Perhaps they nadir slower. The problem is implants don’t have high nadirs at 1 yr and in my database, 90% of that 1 yr data is complete - it may move some but not enough. And now with time, I treat this men with 7250/29 and they are not mirroring the SBRT cohort.
A difference in the radiobiologic effects in prostate cancer such that I’m seeing an exaggerated inflammatory type response with these very high doses via SBRT. And maybe that effect is more pronounced with proton therapy due to some still poorly understood mechanism with protons and low alpha/beta tumors. Perhaps, but we need more data to support this concept. Again I tend to point to implant data and SBRT data that generally shows lower is better and lower earlier is better.
I’m bad and miss prostate - again, I don’t think so. :) I think the intermediate group of 80+ patients with a very low year 1 nadir argues strongly against that. This is same target, same volume. Essentially all other variables removed but dose.
Margins were changed. I DID adjust margins by 1 or 2 mm with SBRT after the higher initial toxicity - trying to simulate IMRT dosimetry a bit with USPT planning 38 to CTV and 40 to GTV. My standard PTV margin is 5mm and 4mm at the center. So here I’m closer to 3.5 mm and 2.5 mm with tighter block margins - fids and daily imaging of each field in really low ECE risk group patients - I do not believe this is the reason for the difference, but trying to write down all options.
And so, the Deeper Dive into the Data Begins:
My personal 25 yr clinical history is based largely in traditional fractionation. We have vast masses of data, but as I showed earlier (Can we de-escalate better), it is all amazingly consistent for prostate cancer in traditional, hypofractionated, and even LDR and even HDR after some initial kinetics that are likely procedurally related.
But at least on my initial review of the literature, SBRT seems less so. Doses vary a LOT. Some results are outstanding but others, less so. Huge multi-institutional data looks SUPER - nadirs that simply are NOT achieved with IMRT. But then Fox Chase and my own experience point towards something different. And then I call people and find out I’m not the only one who think like I do - for a couple of years - PSA kinetics ARE wonky and not as low with SBRT. We have uniform dosing vs non-uniform approaches. A lot of variables at play and simply a lack of consistency.
All of that to say that I simply have questions. I’m not for or against SBRT. If it improves cure rate with manageable toxicity, I love it. If the FLAME approach with SIB or external + brachy or protons are the best answer - that is what I will recommend. I like prioritizing cancer outcomes over number of treatments. As I’ve said, SBRT has been a wonderful approach - likely the single largest improvement in two decades - but it is great because it dramatically improves outcomes. Not because it is shorter.
As I said earlier, I do believe my treated group will ultimately have a very high cure rate - they simply had minimal disease. But if SBRT causes 2 years of drama as we worry about PSAs compared to longer courses of 29 fractions AND it comes with even a bit higher toxicity rate, I don’t like it. And if I’m going to roll this out in higher risk men with PSMA scans out there in the community, I really don’t like 2-3 years of questioning and concern when it might be PSA kinetics. That is not a good path in the US healthcare system where over treatment and too many procedures are a real issue in my assessment. Even a few extra biopsies seems to be an unwarranted risk.
I don’t have answers - I’m looking for them. I believe the answer is in the nuance of planning and delivery and dose gradients across the target volumes and the chosen prescription dose. But that concerns me when we are really advertising that SBRT is the path for all prostate cancer (this is what we post routinely on social sites). As I described previously, we used to really worry about rolling out specific regimens, now we seem to have less concern.
So from here, with the context of why that hopefully you now understand, we’ll begin to walk through data and point out the good and, to me, what is inconsistent. If you want consistency, go back to my reference article on “can we de-escalate better” and read through those 20+ references - there are NO big outliers. In general prostate cancer response is consistent and predictable. I do not believe that fact will change with SBRT.
And you believe I’m missing something, please reach out - looking to learn and be better.
REFRENCES:
Permanent prostate brachytherapy preplanned technique: The modern Seattle method step-by-step and dosimetric outcomes
https://pubmed.ncbi.nlm.nih.gov/19433321/25-Year disease-free survival rate after irradiation for prostate cancer calculated with the prostate specific antigen definition of recurrence used for radical prostatectomy
https://pubmed.ncbi.nlm.nih.gov/23103235/Hypofractionated Versus Standard Fractionated Proton-beam Therapy for Low-risk Prostate Cancer: Interim Results of a Randomized Trial PCG GU 002
https://pubmed.ncbi.nlm.nih.gov/26523442/Five- and seven-year outcomes for image-guided moderately accelerated hypofractionated proton therapy for prostate cancer (UFPT)
https://pubmed.ncbi.nlm.nih.gov/34965846/www.protons101.com, home of the original Protons 101 website.
Content for the Protons101 blog written by Mark Storey MD.



