PACE B: 95% Cure Rate at 5 yrs!!
Great Results presented at ASTRO 2023 using radiation for prostate cancer.
Headline Summary:
95% of the time, you can cure more favorable intermediate risk prostate cancer with radiation - a non-invasive treatment. A fantastic cure rate and an amazing achievement. We can achieve that result with 20 treatments and we achieve that result in as short as 5 treatments. Five treatments can now be consider the standard approach if you apply some basic selection criteria (prostate size, reasonable baseline urinary function) and your patients accept a bit higher Grade 1 and 2 bladder toxicity (urgency / frequency type symptoms) and, likely, less clarity on PSA kinetics for a few years.
We’ve talked at length about the study prior to release.
Today, we’ll review what I got right and what I got wrong. With the clear benefit of retrospection, we’ll take a look and give some final commentary on the trial. I’ve included quite a few slides to help try and build a reference document that people can come back to for details.
Just to review basics:
90% were “intermediate risk” but it was limited to a favorable subset - not exactly NCCN favorable, but not low risk either:
T1c-T2c
Gleason <=3+4
PSA <=20, MRI staged
No ADT
69% with PSAs of <10
80% with 3+4 disease
44% with T2c clinical disease
According to the Partin tables - only about 1/2 expected to have organ confined disease based on the above parameters (blended weight gross approximation).
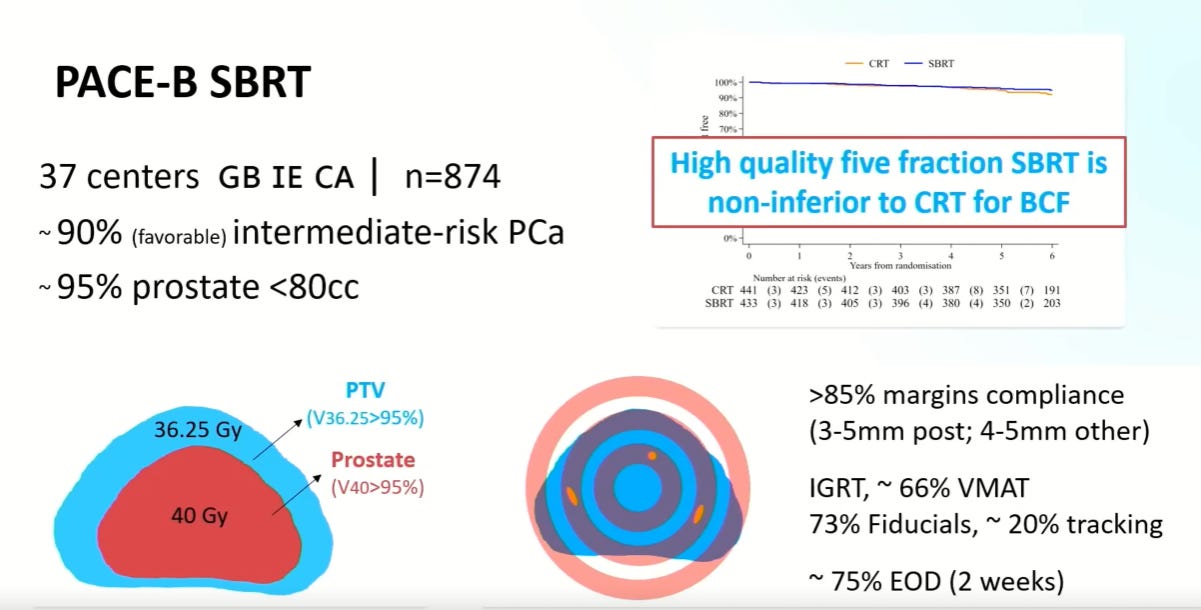
The SBRT arm delivered 36.25 Gy to the PTV and 40 Gy to the CTV.
The trial began in 2012 but a full 2/3rds of the patients enrolled between Aug 16 and Dec 17

With a median follow-up of 73.8 months, the biochemical / clinical failure free survival was 94.6% for conventional radiation and 95.8% for the SBRT arm.
Basically, we cured nearly everyone - in either arm. And follow-up was long at over 6 years. Wow. Hopefully we can simply do away with focal upfront treatments or things like the TULSA-PRO approach that simply do not compare to these results for disease control. Even for surgery, this creates a really high bar. Truly outstanding results demonstrating just how strong radiation outcomes are today for prostate cancer.
Toxicity Updates:
In addition, toxicity was updated to reflect 5 year data. GI toxicity curves looked pretty much identical between the two arms for both RTOG and CTCAE measurements - really no difference so not included.
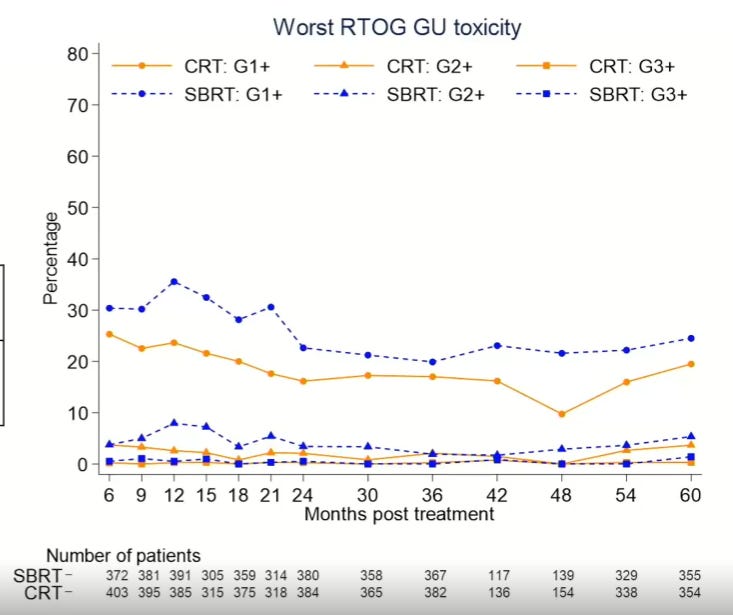
In slight contrast, RTOG GU toxicity is higher to some degree - the p value is NOT significant, but the curves appear different in for Gr1 and Gr2 toxicities. You can judge.
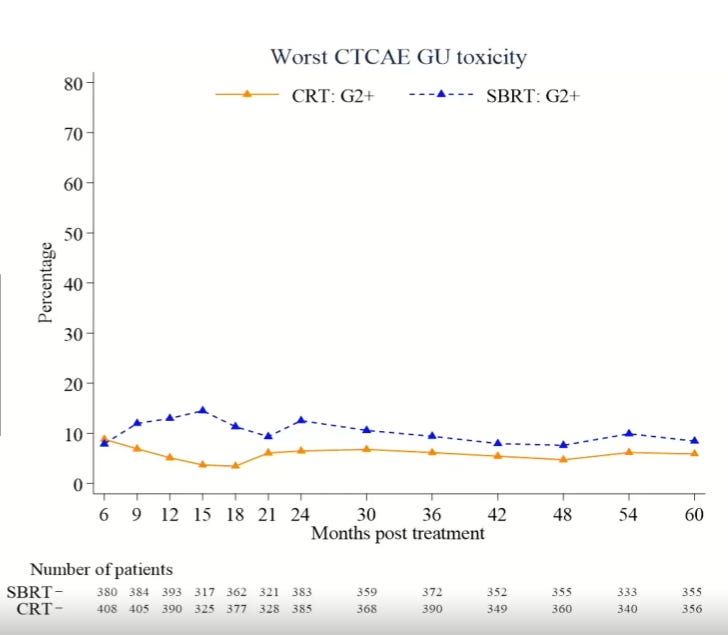
CTCAE toxicity is quite similar with about 1 in 10 additional men having Gr1 toxicity vs. none and about 1 in 10 additional men having Gr2 toxicity especially around the 15 month mark - it moved from 5% to 15% so it does represent a 3x risk at that point and realistically remains at a hazard rate of 1.2 - 1.5 beyond 30 months. On a fixed timepoint, CTCAE is not different but on a cumulative analysis, this difference is significantly different with SBRT having more CTCAE GU toxicity. (data not yet published for this 5 year period - 2 yr data here).
So really it appears that the difference is in Grade 2 toxicity - with at least about 1 in 10 having more symptoms following treatment. In the RTOG toxicity curves, the rate of Gr2 toxicity is still about about double the risk for the SBRT arm at 4 years following treatment. 9 of 10 men will have a similar result but for 1 in 10 - they do have more low grade urinary issues.
And remember, there a correlation between acute and late toxicity.
I’m going to come back to some of the late toxicity later as I'm running out of space - it was a separate session - separate talk.
Sunday, prior to the release of data walking around the exhibit hall, I had the opportunity to have a good 5-10 min or so conversation with Dr. Nicholas van As (Medical Director Royal Marsden NHS and presenter of the session) and discuss the upcoming results. I asked him what I think was my biggest surprise - the move of the standard arm to 95% from historically closer to 85%.
In summary, neither of us are sure. Maybe it is simply with modern treatments we missing less or maybe the increase in the number of cores or availability with newer imaging to find high risk disease which then leads to stage migration? Dr. Loblaw makes the comment that PACE reported freedom from clinical/biochemical failure, not DFS. The difference in events is men dying from other causes which certainly has a real effect on the data. I think all carry, at a minimum, real potential.
Regardless, Dr. van As agreed the move to 62 / 20 (instead of 60) might push it a few percent higher - and both he and I expected it to land in upper 80’s, yet we far exceeded that mark. So my expectations were in fact incorrect. Even for the SBRT arm I have 88% written down here on the site - I thought it was 36.25 Gy when I made that pick and might have considered 92% for the 40 Gy that was delivered - but the hazard rate for failure was still nearly half of 92% at 95.8%.
So I don’t have a clear answer. Dr. van As thinks most of the difference is in the lack of nuance in the posterior aspect of the prostate dosing and the fact that today, we are really good at hitting the target. Until someone proves that wrong, that makes sense. Modern radiation is just that good. And yes, I was low and ironically a poll on X / Twitter was correct with 60% saying north of 92%. Call balls and strikes - I was wrong / Twitter poll was right.
Dr. Ale Berlin (Princess Margaret Cancer Centre - that’s in London, I mean Toronto) gave the discussion talk that followed. I had the opportunity to sit with him for about an hour over dinner after that talk and for at least part of that hour we talked about the PACE data and where we’re headed (much of it was more focused on basic geography for my behalf, some business discussions regarding the US market, and Dr. Shankar Siva illustrating his uncanny ability to generate AI art via his phone, but I digress).
Dr. Berlin relayed, he didn’t see much to pick at. He got the data Wednesday and put together what I thought was a very on point and really strong discussion of the trial. Well done! I will say, it is nice to see studies that you had the opportunity to work on still show up in the Plenary session as he walked through the history of our progress (yes, I was only on the MDACC acute toxicity data - not the results paper, but still…)
And in covering the trial, he really did present a ton of information regarding the approach. Below we review many of the basics of the patient cohort and the prescription for both PACE-B and NRG-GU005

And he did a really nice job in discussing the margins and just how different they were. As he stated, we still don’t have much granular data but this is a graphic he created to scale showing just how different the two arms were. Just taking the mid point for this 50 cc example one would have 110 vs 85 or about 30% more tissue treated in the standard dose arm - from a technical aspect the prescription approach of CTV vs PTV adds at least 1 more millimeter of difference not represented (CRT within dose shoulder while SBRT beyond shoulder).

But throughout both presentations, from my perspective, they each did very well in clearly reviewing the data, the doses and the differences between the arms, even speaking to the nuance I have discussed on this site. Below is a point from Dr. Berlin’s slide speaking to this point describing the SBRT arm as “less forgiving”.
Less forgiving: need to “technically wary” to achieve the presented results.
And on that note, this slide is important - clear descriptions of the OAR constraints.
Finally, this was my favorite quote of the day regarding how we push forward from here:
It is perhaps impossible to think that the collapsing into a two dimensional space with DVH and point criteria will be sufficient to unravel predictors of toxicity in a robust manner.
It likely is the case that we need to start doing more and more voxel analysis in our data - this is where the cardiac data in lung and breast cancer data is headed and it makes a ton of sense to me that these types of approaches will be better able to capture ways to further decrease toxicity moving forward. Perhaps we are getting about as good as we can with these simplistic 2D approaches.
Beyond the Experts: My commentary
My thoughts are this. Nearly 96% is wonderful control in a randomized prospective multi-institutional trial. Yes, minor bladder toxicity is higher but this approach also has clear advantages of efficiency, patient convenience, and lower costs. And remember a significant portion, if treated with surgery, will have adverse pathology features per the Partin Table data so this has really raised standard of care expectations for definitive single modality treatment to a new high bar.
To me, the toxicity data is out there and real for the five fraction arm. Even at 4 years out there appears to be a persistent difference in arms, albeit only seen in Grade 1 and Grade 2. So to me, this shows that realistically, for some men, it is probably reasonable to back off dose in places and move towards the NRG-GU005 dosing or simply give a longer “more traditional” course. NRG-GU005 dosing probably does two things - lowers control just a bit but lowers toxicity - a reasonable alternative option in my mind. At 96% control, I see that as a viable path if needed which adds to the robustness of the five fraction approach.
And a comment on kinetics. Even though not in the results, I sat around tables with very high volume SBRT physicians that evening and at least some acknowledge that PSAs do not drop as consistently for all men with SBRT. That really doesn’t show up in the Consortium dataset that I often refer to, but it is in mine as I’ve reported and it was acknowledged by several people with high volume practices. So I don’t think my data or the Fox Chase data is an outlier. Beyond 2 to 3 years, my data is settling down to low nadirs but it has taken a while. It is certainly something I think reasonable to review with patients regarding expectations - there is a real chance that there is far less clarity with the PSA giving clear feedback with SBRT for the first 2 years.
Those are the two downsides.
That said, this data clearly pushes SBRT as a more appropriate approach for many men - especially those with FIR disease, smaller prostates, and better baseline AUA scores - and data is soon coming for disease up to very high risk cohorts. I don’t think we throw away longer fractionation approaches, but this pushes us pretty far for these more favorable intermediate cases in my view.
And with that needing where we need to go, I’m considering presenting a plan to lay out how I’d transition a more rural practice to SBRT based on my own experience, a number of conversations with various experts, this data, and about 10 months largely in the weeds of the data. I also want to cover the late toxicity data - it has some interesting implications that just don’t fit into today’s document.
Finally kudos to all involved - from the patients to the researchers to ASTRO for the promotion of the science!! It truly is remarkable that we can move from 8 wks (40-45 fractions) to just 5 fractions for so many patients in just two decades. It is a wonderful example of our specialties application of knowledge, use of scientific trials, the implementation of advanced technology and more broadly the value that radiation oncology represents within oncology.