Breast Cancer: Just add Lidocaine?
Yep! Injecting lidocaine in the immediate presurgical setting improved survival.
Certain topics need more urgent coverage - this one breaks up our SBRT prostate series. It is one to know if you work in cancer. To me, the current best argument against the following trial is simply how much it stands out as different. Before we begin let me say, it needs to be repeated. Once repeated, if verified, it is standard of care.
As an introduction, I’ll simply say, this is maybe the most surprising result I can remember - that is in the entire HISTORY of my oncology career.
Effect of Peritumoral Infiltration of Local Anesthetic Before Surgery on Survival in Early Breast Cancer (Ref 1). The trial looked at injecting lidocaine around the tumor in the 7-10 min prior to surgery and it improved survival for breast cancer patients - here are quotes directly from the abstract.
PURPOSE
Preventing metastases by using perioperative interventions has not been adequately explored. Local anesthesia blocks voltage-gated sodium channels and thereby prevents activation of prometastatic pathways….
METHODS
Women with early breast cancer planned for upfront surgery without prior neoadjuvant treatment were randomly assigned to receive peritumoral injection of 0.5% lidocaine, 7-10 minutes before surgery (local anesthetics [LA] arm) or surgery without lidocaine (no LA arm)….
RESULTS
1,583 of 1,600 randomly assigned patients were included in this analysis (LA, 796; no LA, 804). At a median follow-up of 68 months, there were 255 DFS events (LA, 109; no LA, 146) and 189 deaths (LA, 79; no LA, 110). In LA and no LA arms, 5-year DFS rates were 86.6% and 82.6% (hazard ratio [HR], 0.74; 95% CI, 0.58 to 0.95; P = .017) and 5-year OS rates were 90.1% and 86.4%, respectively (HR, 0.71; 95% CI, 0.53 to 0.94; P = .019).
Using competing risk analyses, in LA and no LA arms, 5-year cumulative incidence rates of locoregional recurrence were 3.4% and 4.5% (HR, 0.68; 95% CI, 0.41 to 1.11), and distant recurrence rates were 8.5% and 11.6%, respectively (HR, 0.73; 95% CI, 0.53 to 0.99).
CONCLUSION
Peritumoral injection of lidocaine before breast cancer surgery significantly increases DFS and OS. Altering events at the time of surgery can prevent metastases in early breast cancer (CTRI/2014/11/005228).
(trimmed but otherwise not edited)
Ah… Wow.
For context on scope of this difference, I’ll quote Todd Scarborough - another practicing radiation oncologist from Twitter:
Thoughts for the day: For older women with early breast cancer, lidocaine has a greater survival benefit than radiation therapy For women with N+ BrCA, lidocaine has a greater overall and disease free survival benefit than elective nodal irradiation.
The trial is out of Tata Memorial in India - 20 yrs ago I’d say a largely unknown institution but in more recent periods, they are a radiation trial powerhouse. This is from a leading institution that has been performing standard of care setting trials.
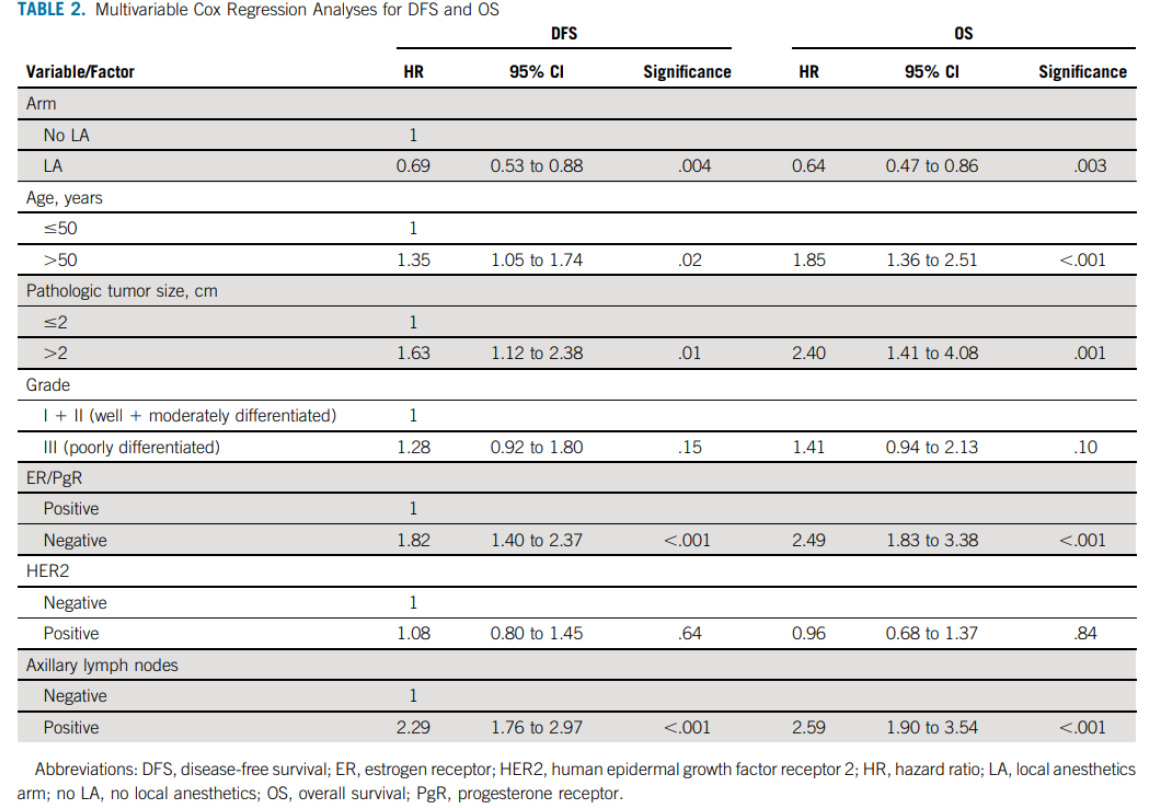
Below is the multivariable analysis for both DFS and OS.
Here are the curves from the trial:
All I can see is that it seems to work. Data is consistent and seems to be a true finding in this trial.
Again - wow. For perspective, this is a greater impact than from anything in the breast radiation literature and on par with the benefit of many targeted breast cancer treatments that cause significant toxicity. This… this is extra lidocaine injected just prior to cutting the tumor out. It has basic science behind the rationale and seems to demonstrate a big win.
A brief history of just how big of a win this is:
Back in the day when I was learning the ropes of radiation oncology, there was a famous scientist Bernie Fisher - he ran the NASBP trials and realistically that group set the standard for breast care for decades. He is known for his unique thinking on breast cancer that I’ll quote and then paraphrase below.
Bernie Fisher: “Variations in local-regional therapy are unlikely to substantially affect survival.”
Or in my laymans terms from a radiation oncology perspective: The destiny for the patient was largely pre-determined at a time before surgery.
Mine is an over simplification mind you - but sometimes I’m simple.
And he ran trials - prospective large national randomized trials - some seemingly crazy in design that showed, to many, unexplainable results:
NSABP-04 (ref 2) - Radical Mastectomy, Total mastectomy or Total Mastectomy and radiation - 3 options for node negative and the last two options for node positive breast cancer - NO DIFFERENCE in disease-free survival, relapse-free survival, distant-disease–free survival, or overall survival. At 25 years, no difference regardless of approach.
NSABP-06 (ref 3) - Total Mastectomy vs Lumpectomy alone vs lumpectomy and whole breast radiation. Again, No difference in survival.
The B06 trial showed this massive benefit in the cumulative incidence of recurrence:
And yet survival was the same. Like I simplified to above - the result of the breast cancer was largely pre-determined before the diagnosis. At least with respect to local-regional control. I believe his argument was that it is a systemic disease from diagnosis - you need good surgery with clear margins and then move along - often along a less aggressive surgical path with large more invasive surgeries not adding benefit.
And in the radiation world some of this didn’t sit well. How could such a huge reduction in local recurrence not affect survival? That is what we do - we reduce local recurrence to therefore improve the chance of cancer coming back which should lead to better survival.
And then in 2000, there was a meta-analysis that seemed to make more sense (ref 4) - yes radiation reduces local recurrence and then if you only had enough women in the trial it would demonstrate an effect on overall survival. The B06 curve above simply can’t be right - no way you can go from 40% recurrence to 15% and not see a reduction in deaths - not possible. At least that seemed to be the thinking and finally this meta-analysis showed the “truth”.
At that time in our field, there were hints / suggestions that we were causing cardiac disease back in the day (like in the 80s) - the argument being we were winning on breast cancer but causing enough cardiac mortality to offset that “win” - how else would this make sense. And now, “in 2000”, with improvements in technique you lessened the negative and could see the benefit of radiation - at least that was my memory of our history as it was taught to me.
But lets be clear - NO prospective trial to date has shown any OS benefit to radiation in node negative breast cancer. Not the old ones and not the new ones: NSABP-21, Canadian Trial, CALGB 9343, PRIME II - no OS benefit. The benefit is in local control (ref 5).
Radiation DOES improve Local Regional Control and that is important in avoiding retreatment and recurrence. But OS for node negative women - I believe that answer is best answered as no. I have two breast semi-related articles on this Substack currently (here, and here if you are interested)
Compare that to this Overall Survival graphic from this lidocaine trial:
Simply: Wow. (third time, I know but warranted.)
That something so inexpensive and so easy that has been around so long could impact outcomes so dramatically is difficult to grasp. It is a headline win in the abstract and a subset / multi-variate analysis win as you look deeper. Heck, it even worked to inject lidocaine and then do a mastectomy.
And realistically, I don’t think it is inconsistent with what Bernie Fisher proposed. On some level, the lidocaine is not an adjunct local treatment, but it is acting via known pathways to inhibit metastatic spread - a local treatment with the ability to affect the systemic metastatic potential of the cancer. Brilliant!
Today I had two old memories:
The no touch technique - back in the day, especially in rectal cancer there was a “no touch isolation” surgical approach. It gained enough momentum that they ran trials comparing surgical approaches - ultimately it wasn’t deemed an important difference. But I laugh today as it is pretty much this approach - limit spread at the time of surgery - the older method applied a manual / physical approach and this new one uses a drug / pathway / chemical approach. Full circle. Reference is from 1988 - I’m not that old, but I remember the history that old :) (ref 6).
A quote to me from an old breast surgeon - Kent Westbrook. He learned I was going into radiation and he looked at me and said, “radiation works best when you don’t need it.” Probably from around 1995. Haha. First time in over a decade I flashed to that quote.
There is an editorial to the article here (ref 7). It is very well done and I won’t summarize it here. It points out, largely like I do, the uniqueness of the results. If you wish to pick at the trial and attempt to argue against it, it is a good read. The main argument against the trial it that it was slow to accrue and ultimately the criteria for “success” was altered. By some measures, it is therefore technically negative. It also quite nicely discusses that surgery was up front whereas in the US many of these women have other neoadjuvant treatments that might minimize or negate this effect.
As we touched upon at the opening. Due to the divergence from our history, this needs to be replicated. Flip a coin a million times and you’ll get some weird streaks - some “picks” the lottery numbers - crazy things happen statistically even in prospective settings. To me, this is as strong an argument as anything I see in the editorial.
And ultimately the editorial lands where I do - this seems like we need to figure out how and why exactly this worked so well and if it is reproducible.
And if it works in breast cancer, can we use it in other places, with other tumor types to improve cancer outcomes. Exciting times, from a vial of 0.5% lidocaine - who would have thought?
(The Answer: At least a few scientist in India, and not just thought about it but developed the trial and then performed the work to carry the trial out to its conclusion - Kudos!!).
As always, author of one - if I missed something in this rapid release or you read something different, please comment or reach out.
REFERENCES:
Effect of Peritumoral Infiltration of Local Anesthetic Before Surgery on Survival in Early Breast Cancer
https://ascopubs.org/doi/abs/10.1200/JCO.22.01966?journalCode=jcoTwenty-five year follow-up of a randomized trial comparing radical mastectomy, total mastectomy and total mastectomy followed by irradiation
https://www.nejm.org/doi/pdf/10.1056/NEJMoa020128Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer
https://pubmed.ncbi.nlm.nih.gov/12393820/Does locoregional radiation therapy improve survival in breast cancer? A meta-analysis
https://pubmed.ncbi.nlm.nih.gov/10715291/Which Patients With Breast Cancer Can Omit Radiotherapy?
https://ascopost.com/issues/april-10-2023/which-patients-with-breast-cancer-can-omit-radiotherapy/No-touch isolation technique in colon cancer: a controlled prospective trial
https://pubmed.ncbi.nlm.nih.gov/3292002/Peritumoral Lidocaine Injection: A Low-Cost, Easily Implemented Intervention to Improve Outcomes in Early-Stage Breast Cancer
https://ascopubs.org/doi/10.1200/JCO.23.00418www.protons101.com, home of the original Protons 101 website.
Content for the Protons101 blog written by Mark Storey MD.