Breast Cancer, Radiation, and Heart Health: (PATIENT ADVOCACY SERIES)
Today is a breast cancer advocacy piece. We'll discuss what patients can control if diagnosed with breast cancer to reduce their risk of cardiac disease.
My initial self-publication goal for the Substack was 20 articles - start there and see what happens. And with surpassing 20 quite early in the year, I wanted to do a patient / referring physician type article. Less technical than most posts will be on this Substack. And just for note and context - this includes the context of the data of the Feb 13th, 2023 NEJM article (ref 1) where some women who are older and have early disease might be able to avoid treatment very safely - so it is all up to date.
In 2018 the American Heart Association released its first official scientific statement regarding heart disease and Breast cancer.
The first line of the conclusion of this statement is shown below (ref 2):
Conclusions
Ideal breast cancer outcomes are reliant on coexisting cardiovascular health along the entire journey of breast cancer treatment.
My version is something like this:
Protecting the heart during breast cancer treatment is a critical component of a successful treatment plan.
Before we start the more technical side of the discussion, I’d like to remind everyone of the basics of heart health. These are critical. Don’t let the fear of a cancer diagnosis sidetrack you from the basics. While there are many things you cannot control, focus on the simple things that you can. These items are available to everyone and are actionable steps you can take towards long term heart health:
Actionable items you, the patient, can control:
Stop smoking
Eat a healthy diet
Stay active and exercise during and after your treatment
Be active in managing blood pressure, cholesterol, and diabetes.
These are very important. They are items that you can control. In fact, they likely have more impact on your long term cardiac health than anything else in this review.
The other main point to remember is:
For many breast cancer patients, radiation likely improves survival. It is often a critical component of your treatment even though it has side effects. For those with the earliest and most favorable cancers, it often still dramatically reduces your risk breast cancer recurrence.
Keep it simple. It is ok to look at details, but if you are overwhelmed remember to back up and consider the above simple statements.
EDUCATION:
The 5th controllable item is to be informed / educated. This allows you better context to follow the discussions that will happen at seemingly breakneck speed (while your physician likely feels like they are going very slowly). It allows you the chance to possibly anticipate the discussion and then be more interactive during the process. You can be better informed to listen for specific words or terms. Ask better questions and get better information about your case. So today, we’ll touch on a few basics.
While we have lots of great treatment options for breast cancer, there are actually several important treatments that have KNOWN significant heart side effects. In fact, if you are 65 years or older when diagnosed with early breast cancer, the predominant cause of mortality is heart disease and not breast cancer.
We’ll just focus on a few breast cancer treatments below that impact heart-health:
Adriamycin - a chemotherapy, sometimes referred to as the “red-devil” in infusion suites (chemo rooms). The main toxicity of this drug is heart damage which can lead to congestive heart failure. It is a great drug for many women and improves survival for women with breast cancer, but definitely affects the heart.
Herceptin - (or trastuzumab) this is a newer targeted treatment against cancers that over express the HER2 gene. Again, it is a great treatment for some women but unfortunately the primary side effect of the drug is cardiac toxicity with a risk of congestive heart failure.
Radiation - Radiation dose to the heart causes long term damage on some level. There was an important study published in 2013 showing that for every 1 unit “Gy” of radiation delivered to the whole heart, the risk of a significant heart event increased by 7.4%. So if your heart receives 4Gy, then you have a ~29% greater chance of a significant heart event (ie heart attack that put the patient into the hospital or heart attack that resulted in death).
(note: 29% greater works this way. If your 10 yr risk of cardiac disease is 10%, then according to this study, if your mean heart dose was 4Gy, you would have a 12.9% risk of cardiac disease - not 10% + 29%)
Note: Surgery is not in the list - it really does good at not causing long term effects on the heart or lungs.
The three above treatments are recommended when we believe they improve your outcomes from your breast cancer even knowing these risks. In cases, your physician will discuss with you options (if you’re on the edge of benefiting from a treatment like chemotherapy or not), and in those cases, you do have some input, but for many cases, the requirement of these three items is beyond your control.
As I often say, the ideal answer is not having the cancer. Once diagnosed, we now have to look at what we can do with where we are today and figure out the best plan for you.
WHAT YOU REALLY CAN’T CHANGE, THE RISK FROM ADRIAMYCIN AND HERCEPTIN:
Realistically you can not change the need for these components - many women simply need these components for their treatment. They can be critical pieces to the successful management of breast cancer. Adriamycin and Herceptin risks are largely not changeable by the patient or doctor. As the doctor, you can perform heart imaging to try and pick healthier patients for these drugs but we really can’t alter the risk if these treatments are indicated. Remember the context PLEASE, these drugs even with side effects - help cure / control the breast cancer and can lead to LONGER SURVIVAL.
What you can change on some level: radiation dose to the heart.
From my perspective, this is single area where a patient MIGHT be able to have some impact. And I don’t think it is complicated.
Ask your doctor about your radiation plan and talk about trying to limit your heart dose.
That’s it. I’ll give a few more details but simply asking the question and discussing your concern over heart dose probably is the simplest, largest benefit approach.
Before we go further:
Tangent breast cancer treatment is an excellent treatment with very little toxicity and overall survival benefit for many women. When paired with things like surface guidance and or breath hold approaches, tangent treatment is the treatment of choice for the vast majority of even left sided breast cancer patients.
What are type of plan information is relevant:
To me, the two easiest metrics to ask your doctor about are:
Mean heart dose - lower is better. I generally achieve a mean heart dose <1 Gy.
Dose to the LAD (left anterior descending artery) - This is one step more complicated - The volume of that vessel receiving 15 Gy should be less than 10%. It is technically written as v15<10%. So a LAD v15 of 16% is high. A LAD v15 of 8% is in the low / ideal range.
If your plan meets these two metrics (or is very close), then your plan is really, really low risk to cause heart damage.
IT IS NOT A SIMPLE ONE WAY STREET. LESS RADIATION DOSE TO THE HEART CAUSES LESS CARDIAC RISK, BUT YOUR DOCTOR MAY BE COMPROMIZING / DECIDING BETWEEN HEART DOSE AND COVERING AREAS WHERE THE BREAST CANCER CAN RETURN.
This is where, on a national level, we are looking at proton therapy. We are evaluating in trials whether protons have a role in more advanced cases - specifically when the IMC lymph nodes (lymph nodes behind the sternum) will be covered is the primary area of interest. The idea is protons offer less compromise of areas at risk while keeping heart doses lower. To date, there is no clear proven benefit, but there is good data supporting this large national trial - the RADCOMP trial.
WHAT IF PROTON THERAPY ISN’T AVAILABLE IN MY AREA OR MY HEART DOSE SEEMS VERY HIGH?
Protons are not a magical fix. The current trial may or may not demonstrate real measurable improvements - many, like myself, think the odds are in favor of protons to help some women, but there are many bright educated physicians who do not believe that will be the case. Until the large RADCOMP trial is completed, we don’t have a precise answer.
(Trial participation is always encouraged if you are interested. It helps us define the best treatments today for the patients of tomorrow. Simply being enrolled on a trial has been shown to improve patient outcomes - everyone knows the results will be examined and that pushes people in the correct direction - in many ways, similar to simply asking about heart dose.)
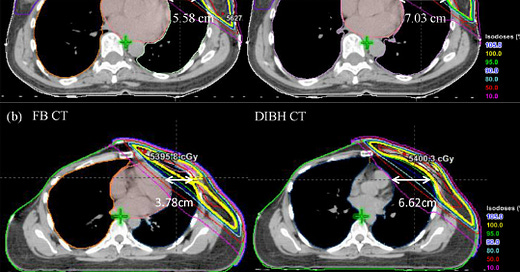
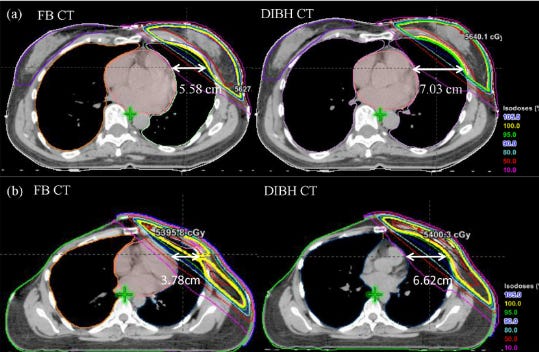
There are other paths beyond protons to decrease heart dose. The main approach these days is to use a breath hold technique. The patient takes a deep breath and holds it. That pushes the chest / breast up and away from the heart and gives more room for the physician to design your plan without treating the heart. It is shortened to DIBH (deep inspiration breath hold) and can use IGRT (image guided radiation therapy) or Surface Guided Radiotherapy (where cameras monitor your anatomy for motion). It can be used with IMRT (intensity modulated radiotherapy) to help “bend” the radiation off the heart and coronary vessels. These are just some of the approaches. An example of the difference DIBH can make is shown below.
There might be longer-term preventative options:
Some clinics are building Cardio-Oncology clinics. These are specialty clinics where physicians attempt to minimize long-term risks from any cancer treatment that relates to cardiac risk. They will certainly cover the main actionable items, but they might have more information to help reduce your long-term cardiac risk beyond these simple steps such as more frequent scans and up to date medical recommendations. I do NOT think these substitute for lowering treatment risk, but they CAN help you to optimize your options following treatment.
Quick story: I work at a large proton center and we get calls from all over the country. A patient was at a big institution elsewhere and her heart dose was over 1 Gy. They weren’t using breath hold - it was available. They weren’t using protons - they were available. She was young with heart disease in her family but they did make a referral to a cardio-oncology clinic to consider long-term statin use. In my opinion, that is the wrong approach. Fix the problem - adjust the plan, use breath-hold or whatever is needed to minimize heart dose AND THEN consider a statin if cardiac treatment related risks warrant the risks of long-term statin use. Don’t do “good enough radiation” and then think taking a medicine likely for decades is the fix. So being involved and asking questions can in fact help improve your treatments. Her plan was adjusted and she did well with treatment and should do really well in the long-term. Crazy things happen daily.
If you asked questions and have had discussions, you have done well.
AGAIN REMEMBER, even in situations where we can’t quite meet the above 2 goals, THE BENEFITS OF RADIATION OUTWEIGH THE RISK OF THE TREATMENT. Don’t let anything here let you think you can avoid radiation if it is recommended by your physicians (some can but many can’t). It has a SURVIVAL BENEFIT in many cases even with the heart health risk. It is more important for younger women with the most aggressive cancers, even though that is where avoiding the heart is most difficult.
Finally: Don’t delay.
Ask your questions early. Radiation needs to begin in a timely fashion. If you find out, for example that your heart dose is higher, but your treatment starts tomorrow, it is probably worse to spend a month to get to a different center, re-start the process, to see a slight reduction in your heart dose. Delays or breaks in your overall course of treatment should be avoided. Ask questions early and if you wonder about a second opinion, get it sooner rather than later.
In closing:
Be an advocate for your own care. Be informed and ask questions about your heart dose and don’t be afraid to push for better. Control the controllable and press forward as a breast cancer survivor.
REFERENCES:
Breast-Conserving Surgery with or without Irradiation in Early Breast Cancer
DOI: 10.1056/NEJMoa2207586Cardiovascular Disease and Breast Cancer: Where These Entities Intersect: A Scientific Statement From the American Heart Association
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000556