ASTRO Workforce Analysis: Pressures Unique to our field
The ASTRO Workforce Analysis was just released. We'll look at issues I think are a bit unique to our field of medicine.
Being a proton blog, radiation oncology and business intersect. Today, we’ll look at my perspective on issues related to the recent ASTRO Workforce Analysis. Kudos to those who worked hard to bring it to fruition. Your work is appreciated.
I’ll present two clear and specific regions where I think we can make structural billing improvements to help offset the rapid changes in our field. I see them as ideas and proposals - by no means “answers”, but we need to use this opportunity for discussion for how to improve moving forward.
The ASTRO Workforce Analysis
Workforce issues are not unique to radiation oncology:
There are problems in general across medicine. As in many place across the US workforce, there are pressures to increase productivity and struggles with increased regulations and, specifically in the practice of medicine, insurance hurdles that can create massive volumes of work. These are common issues across healthcare and more broadly throughout all of industry.
But radiation oncology has additional issues that are rather unique to our field - not all exclusive, but often more pronounced in our specialty. I think of them as multiplier effects. Today, I just want to review my perspective on history.
Concerns about the future of radiation oncology are not new. They were around with a pretty depressing forward looking analysis back when I was interviewing in 1996. But there have been changes to our field which DO impose real changes to the workflow and workloads of the physicians in the marketplace.
In the summary conclusions of the ASTRO Workforce Analysis (ref 1), they point to a “relative” balance of physicians looking ahead to 2030. Back in the day, I think we graduated less than 120 and today we graduate 175 or so (high was over 200). Our programs have grown significantly over the past two decades. We are clearly an outlier in this regard and it is acknowledged in the review:
Specifically, in the United States, residency positions have rapidly and significantly increased over the past 20 years, triggered by factors, including (1) increasing use of advanced technologies (e.g., intensity modulated radiation therapy), which have resulted in higher reimbursement and technical and professional compensation and (2) the prestige of having or growing a residency program as well as increased clinical support for departments
And it is demonstrated in the graph below where, related to other medical specialties, we are “winning”!!

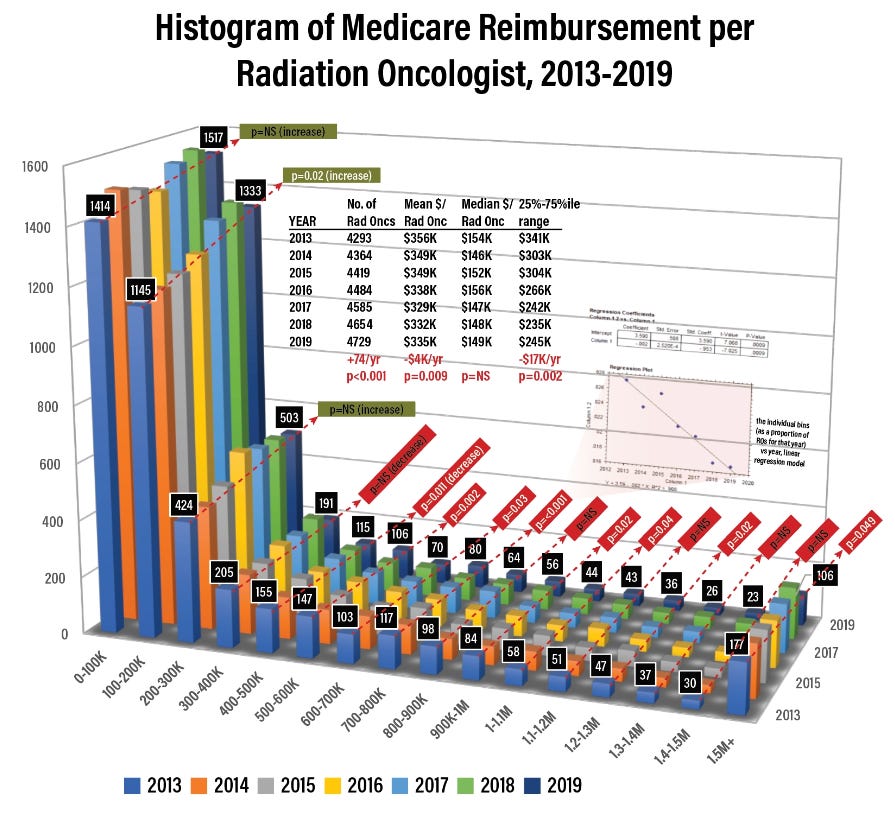
But the statement about IMRT increasing physician compensation is less than fact in my assessment. What I’ve seen over the past 15 yrs or so is more wRVUs required per MD to maintain income at a given level and that YOY trend is increasingly greater in the past few years. This is similar in nearly all medical specialties, but I do think we have unique modifiers which I will discuss.
(nope, no pity parties - at least from me - blessed to have stumbled into the spot)
There is overall pressure on the field and it is quite obvious. We’ve seen a vast jump in unmatched positions via the Match and it was obvious enough to FORCE a decline in total spots from 207 to 176. In just 3 years, 15% of program slots have been removed and still we do not come close to filling via the Match.
If everything was running smoothly for the specialty you would not see large unfilled spots and a pretty dramatic decision by leaders of programs to shrink residency programs. Just would not happen. Our days as one of the most competitive fields top to bottom in all of medicine are, at least for the moment, behind us.
Finally, to set the table for our discussion, the ASTRO Workforce Analysis did not include technical revenue. I think the decision to not evaluate the far larger technical side of revenue is a poor one.
But what I don’t want to do is re-analyze the ASTRO Workforce Analysis, I just want to set the table and point out there is really pressure and that the formal analysis is a partial analysis at best due to lack of consideration of all revenue. I think it is quite evident based on the above information that there are issues despite a (my opinion) very laissez-faire “relative balance” conclusion.
And now we’ll look at my perspective of things that have changed since 2000 that didn’t exist before.
These are pretty obvious but they are real effects:
SBRT:
The GREAT thing about this trend is that patient outcomes improve. This is why this approach is a home run in so many places. But it begins to completely restructure the business model of radiation - not bad or good, but it is drastically different.
In 2015 for example 32.5% of my Medicare income was from weekly management codes (ref 4). Planning and block codes were 2-4 in order of reimbursement and in total about the same percent as weekly management. 5th was E&M visits at 6%. In the SBRT setting 32% of income gets slashed - not to zero but to far less.
(can’t say exactly how much because it depends on your current reference pt population and fractionation, but likely drops to at least 1/3rd of these 2015 percentages)
And yet, from a clinical perspective, risk increase dramatically with SBRT. Supervision time and requirements for oversight are exponentially different. The complexity and time to plan increases. There is literally nothing easier with this shift and yet wRVUs likely drop significantly. Almost as importantly, you can’t easily estimate the impact without a review of exactly what your practice looks like - it is more complex to model than hypofractionation where one can, if one chooses, mentally tabulate the effect.
The payment shifts with SBRT are so dramatic from a global perspective that RO-APM can be manipulated quite significantly jumping to all SBRT models with low capital costs machines - which I don’t believe is the intent.
Hypofractionation:
Hypofractionation again attacks the same revenue stream. It is far less of an effect and can more slowly be implemented so that changes are less clearly felt, but it is there. And today daily imaging codes are not insignificant and these fall as well.
Worse yet, hypofractionation, in general does NOT improve cancer cure rates. From my perspective it has 3 main benefits:
Facility throughput - I believe most interest began in countries needing more throughput due to lack of capital or physician shortages relative to patient bases. Examples: UK or Canada or India
In the US, large referral hospitals can no longer expand in their local market - they have all of the local patients “captured” - what is left is to grow the market often lies beyond 1-2 hours and this is easier to capture those patients when treatments are shorter. Back to my boardroom discussion - the entire roll of the CEO is basically to grow the business.
Increased patient convenience. I see more posts about it helping people in big cities due to traffic, but coming from Arkansas and Oklahoma there are people with literally NO options within 2-3 hrs. It certainly has benefit to some who would not otherwise be able to have treatment.
That’s it. And, in my opinion, leadership combined #2 and #3 into a “Choose wisely” marketing campaign and the specialty at large supported it. Rightfully perhaps as the US was moving very slowly towards less fractions. But I think many were frustrated with proton facilities being built for prostate cancer with large marketing budgets and Urorad facilities with 100% urology ownership treating to 45 fractions taking significant revenue out of radiation oncology. For whatever reason, it was broadly applauded because physicians who both directly benefited (large referral centers) and those who more indirectly would be harmed in the long term (community physicians) saw a way to fight back and impact patient care. Again we do SBRT DESPITE loosing a ton of revenue because it is better for outcomes. (one person’s perspective)
Non-Inferiority has leaked into Radiation Avoidance:
I wrote about this earlier. Our own attacks on our specialty: either costs or “too many fractions” or boisterous disagreement with large capital investments has crept into a broader view of our specialty questioning its value benefit. We now find ourselves beyond just reducing costs to radiation, but being substituted entirely by more costly medications or avoidance in a search for “better” outcomes. I won’t belabor this again, I’ve covered it previously.
A Decade or so of push towards research:
My perspective, but for a time we pushed too hard in the direction of MD/PHDs that really wanted to do lab based research. Probably still today, it is likely really, really hard to match at a top program without a real basic science tilt. I would have been lucky to get into med school never the less a top program.
This push is fine - we need that work to be done, but it also lends to everyone of those physicians wanting to stay at a major academic institution with the complex tools and assets needed to run basic science labs. When in reality, I believe, we need a better blend of people across the country to deliver care. (Again, just see the pendulum swing back towards the middle.)
And again, it serves the entities driving the ship. It creates huge competition for the largest institutions and pay can therefore be kept lower. It opens the avenue for fellowships etc. that did not exist 20 years ago which push payment scales down. It creates physicians with quite limited job options beyond their own systems due to very specialized interests. Simply, it helps to drive these institutions forward.
Capital Costs are massive and payments have shifted in that direction:
And the final rather unique issue is our capital costs. You cannot leave training and decide to go by a MRI linac like you used in school and go set up shop building a 20M+ facility (at least most can’t). You can’t even go to a hospital with an idea for a facility unless you have a 2-5 yr time horizon. What jobs are available are available.
Pair that with a general decline in professional to technical revenue. It used to be that the ratio of professional revenue to technical revenue was say over 25% of global billing. Then it went it 20% or so. In an IMRT prostate only Urorad setting it was around 15% and in a proton center, it is well less than 10% and likely <5% at many large institutions due to technical payment rates often in excess of 100k.
Fractions are the first multiplier and this is the second. It works both ways if you know your stuff. They need you to unlock the revenue in sparsely desired regions but in competitive markets, the lower your value ratio, the less valuable / more replaceable you become.
The ASTRO Workforce Analysis addresses some of these issues and from my perspective others are essentially ignored due to an avoidance to consider technical revenue. There are some real pressures on the industry. It is why I write about our need to re-focus on optimizing treatment and embracing technology.
My Suggestions:
Address SBRT and the effect of weekly management codes dominating wRVU:
I’ve written before on the importance in trying to swing the pendulum back towards the middle on fractionation and technology - a refocus on cancer outcomes. We are making strides in shrinking the number of residency slots and that is progress. The fact that ASTRO and the physician leaders on this project did put such a large volume of work into this project shows signs of improvement as well. So in places, we are making changes.
At the same time, some of the items that I list above are simply facts. I don’t think we can address the cost of capital issue. In fact, I argue on this Substack, that we continue to rely on this very equipment and it is the foundation to our specialty. It is very unlikely in the next 10 years that we see the capital costs see dramatic decreases - rather I think the global professional to technical ratio continues to decline and I don’t think this is addressable on any significant level.
But I do think there is one addressable issue that we are not / and have not elected to address. The importance of the weekly management code to ultimate professional revenue. It sits at the center of the issue regarding the decreasing number of fractions leading to less revenue and then the struggle to maintain incomes - it is one of the multipliers to the downward pressure on income in our field that is rather unique to our specialty. Further it sits at the center of such stupid results of the RO-APM model reimbursing prostate cancer at 50% more than a breast cancer (ref 3). That is largely this single code and legacy 8 weeks of treatment bundled into our “new age” payment model. Yet it has continued to be a centerpiece and unchanged for the past decade during our push to decrease fractions.
On possible proposal might be simply shifting this code to a per treatment course approach. If you set a per treatment course flat rate (just taking RO-APM professional payments as a reference) at ~$730 ($2250 x 32.5% - taken from my own stats above) it would negate the effects of decreasing fractions. If you then wanted to prioritize hypofractionation, you could set a multiplier of 1.1 as an example to push in that direction giving reimbursement of ~$800 in a low fraction scenario. It would be the opposite end effect of what we see today. It would balance the inherent craziness between prostate and breast cancer payments. It relieves the future pressure that we all see coming with shorter and shorter fractionation schedules on the horizon.
SBRT already has a bump in the weekly management fee - and being just 5 treatments or less - it is essentially a per treatment episode code. I still think, even as structured, the volume of work and toxicity risk is underappreciated and it should be significantly revenue positive for a physician based on wRVU to opt for SBRT. Simply it is more work.
SBRT wRVU adjustment could handled with a multiplier off the global base above or I believe we should consider an additional code for the requirement of supervision at the treatment machine similar to, but in addition to, IGRT. This is real time spent monitoring treatment and begins to account for the toxicity risk of the treatment and the consequences of any misadministration.
In Closing:
I do think we’ve made progress and are slowly shifting towards a new heading. But changes to our field in fractionation are seemingly outpacing our changes especially on the billing / revenue side of the equation. For a number of reasons, in 10 years the coding changes will make less of an impact, but I do believe that ASTRO should seriously examine the impact of weekly management today. Medicine is complex and the transition to single payment per episode of care will take years and in the meantime, we can make progress and address the addressable.
I love the specialty. It IS one where you need to understand that your ultimate job choices are limited and that job searches will cover (by necessity) a large portion of the country. But if that is ok for your circumstances, I still believe strongly that it is a great place to be impactful in the lives of cancer patients. We still have much to do to improve the lives of those who need our services as we push forward in search of better.
REFRENCES:
The American Society for Radiation Oncology Workforce Taskforce Review of the United States Radiation Oncology Workforce Analysis
https://www.redjournal.org/article/S0360-3016(23)00207-9/fulltext#tbl0001Unfilled Positions in the 2022 Radiation Oncology Match: A Reduction in Positions
https://www.sciencedirect.com/science/article/abs/pii/S1879850022001254Impact of Radiation Oncology Alternative Payment Model on Community Cancer Centers
https://ascopubs.org/doi/full/10.1200/OP.21.00298Medicare Unmasked
http://graphics.wsj.com/medicare-billing/Image Credit: Diplomats and Reimbursement work care of: https://twitter.com/toddscarbrough