ProtecT: 15 yr results! Great science! But does it translate to the US?
In the US, we expect treatment and expect treatment to make everything better. Patience is not a strength of our system.
Fifteen-Year Outcomes after Monitoring, Surgery, or Radiotherapy for Prostate Cancer
On March 11, a 15 yr update of the UK ProtecT trial was published (ref 1). It enrolled 1643 men to three options:
1) active monitoring
2) prostatectomy
3) radiation
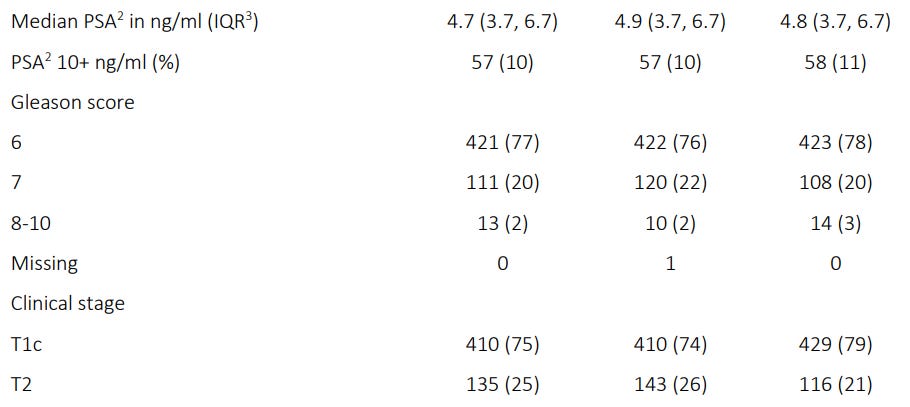
From the abstract, “While most were low risk, over a 1 in 3 had either intermediate or high risk disease.” But realistically a rather low risk cohort - median PSA<5, 10% PSA over 10, 2% Gleason 8,-10 and all T1, T2 disease.
After 15 yrs there was no difference in overall survival. There was more metastatic disease in those who were managed conservatively - basically it doubled from around 5% with treatment to 10% without treatment and there was about a 5% jump in long-term ADT usage from ~7.5% in the treatment arms to ~12.5% in the active monitoring group.
Below are the Primary and Secondary Outcomes as well as important curves.
By the end of the 15 yr follow-up, 1 in 4 had avoided treatment - but looked at differently - 3 in 4 did have treatment in the 15 yrs.
Here is an old infographic from the 10 yr data (ref 2) - basically the trends continued. At 10 yrs, in the UK half will need treatment and by 15 yrs 75% will need treatment - good numbers to discuss - if they apply here.
And 12 yr outcomes document expectations with these treatment approaches (ref 3).
Again Kudos to the authors!! Great trial! Great science! Great accomplishment to complete such a seemingly impossible task - to randomize between following, surgery, and radiation.
But in the end, how will this work and would it really even apply in the US?
The UK and US are very different markets - below we compare and contrast the path of a low risk patient on the ProtecT trial to US NCCN Guideline medicine.
Both are biopsied in 2016 - PSA of 6. Today, PSA is 19. A slow patterned rise.
ProtecT:
Lab only.
US NCCN Version:
MRI in early 2017.
Confirmatory Re-biopsy in late 2017 - required.
Annual MRIs because of rising PSAs
2019 - 3rd biopsy of prostate - periodic biopsies recommended for most men.
2019 - Oncotype due to availability and no prior genetic testing. Still low risk disease.
2022 - 4th biopsy - PSA now above 15 and MRI showed enlargement of lesion.
2023 - recommending 5th biopsy as PSA approaching 20.
I want to emphasize the above is COMPLELELY consistent with our NCCN guidelines. It forces men to have treatment in ways. If we want active monitoring to be an option, we have to fix the guidelines.
This is very real. My very first prostate cancer consult after the data was presented. Literally can’t make this stuff up.
I’ll blur lines so none of this is correct - but pretty darn close:
2016 - first biopsy - GG1
2019 - biopsy #2 - GG1
2020 - 1st MRI
2021 - 2nd MRI / biopsy #3 - GG2 / Oncotype obtained.
2022 - 3rd MRI / questioned for consideration of 4th biopsy.
2023 - PSA now up over 10 - people MORE nervous and referred for treatment.
His rate of PSA rise would have NEVER qualified for discussion of options on the ProtecT trial. In total, over 7 years a gain from just over 5 to just over 10. ProtecT required a rise of at least 50% over 12 months to consider intervention.
In contrast, per NCCN, we didn’t biopsy enough - missed that confirmatory prostate biopsy within 1-2 yrs of original biopsy. If only we had done that.
Take that randomized data!. Until we fix the concept that everything in America can be fixed, we are doomed.
If treatment is given half the time by 10 yrs there, here is probably closer to half or likely even seventy-five percent by 5 years. I’m hoping this trial helps to move our needle but simply stated: I’m sure these data do not represent what a patient would experience in the US.
In the US we loose all common sense. Too many providers and too many people wanting to fix everything. I use “active surveillance” more than most. In the state of Arkansas I used to joke it was a race between me and the VA to see who was following more people with prostate cancer. I use "quotes” because I didn’t routinely biopsy men every year or two either. Something had to change before I would jump in with a procedure - no procedure is without risk.
More often it would be the primary physician or nurse practitioner in some other clinic who would be nervous and without a call, send my patients to a new urologist because they “had cancer” and “no one was doing anything.” I was, just it was coordinating a lab draw every 4 or 6 or 12 months. We talked about options and many were quite happy to be followed but it was work. Work on my side to call PCPs and explain that it was ok. Work on the patient side to fight against the processes that funnel these men into treatment.
And now it will be WORSE because PSMA has arrived. It will affect this data in two ways. First on the treatment side, people will have PSMA scans earlier - likely in partnership with MRIs to look for progression - and at some point we’ll find stuff - an increase in the SUV value - a little larger sized lesions, a change from PIRADS4 to PIRADS5. The trends that drive patients towards treatment will be stronger due to better imaging.
And on the follow-up side, it will change the calculus as well. It is more sensitive and we love finding stuff and not missing things. We all know PSMA is going to change things - hopefully we can figure out the science to have it help outcomes, but it is going to cause a lot of worry and work - especially if you can remember to back up and consider theses results and knowing the real answer is that patience is often an underappreciated path.
Second generalized example: Patient about 3 years out from treatment in upper 70’s had a bump in PSA up to ~0.8. Very nervous. I tried both on phone and in person to be a little slower with pursuing imaging / workups - perhaps that is correct, perhaps it was wrong. He and his family met with me and two other physicians and eventually we had a PSMA scan. It showed a single solitary nodal metastatic lesion. That has now been ablated and we are following. Whether this path or a more conservative path in follow-up is correct, I don’t believe any knows at this point. Time and good data will tell.
So when I read this trial I do really appreciate the science. It is a wonderful question to ask and tremendous to be able to answer. But over here - in the land of “we gotta fix this! And now!” I’m not even sure how much many of the findings apply. It clearly demonstrates low risk of death with more conservative management in many men. But ADT, eventual treatments, and even the distant metastatic rate will be greatly impacted by our patterns of care.
In my first patient, I’m not sure that is a “better” path than just treating. Somewhere along the way, we lost common sense. Think of the stress and issues related to the procedures and costs etc. Not insignificant. And if you have to endure that path and eventually get treated, you really haven’t gained much.
This trial will help move us in the right direction and therefore even if we can’t use some of the findings as “facts”, it is a great study. I do think it will move our market - at least for a moment - towards more conservative management being considered. But I don’t think people in the US should quote numbers related to ADT rate or treatment rates with long-term active monitoring. You can quote them, just have a caveat to the patient about just how different the markets between here and the UK.
And if you need to explain just how different they are, tell them to roll a dice and 1 or 2, we do nothing, 3 or 4, we operate and 5 or 6, we radiate. That should make the point.
But Seriously, What are first steps?
I think we need to seriously consider an overhaul of NCCN guidelines for the “Principles of Active Surveillance and Observation”.
Prior to the end of year 1, a mpMRI, 2nd biopsy, or molecular tumor analysis is recommended.
Currently we require a confirmatory biopsy within 1-2 years. - Do we really believe that would improve the ProtecT conservative management arm?
Additional repeat biopsies are considered as well as MRIs and molecular tumor analysis. Does this really seem beneficial within the context of these results?
In contrast to ProtecT where the main driver of decisions was PSA moving 50% in one year, we talk about Grade reclassification as the most common factor influencing a change in management. In fact, more than 2 biopsies are recommended for most men per the guidelines. I agree with the former approach.
So in 5 years with GG1 disease, one would be following NCCN guidelines to have the following:
-First biopsy showing GG1 based on MRI PIRADS4 lesion and PSA 6.
- Order Oncotype confirming low risk
- 6 months later perform and mpMRI (no change from pre-biopsy)
- At 12 months perform the confirmatory required biopsy per NCCN.
- 3 additional annual mpMRIs.
- Yr 3 and yr 5 biopsies for stability of disease
Addressing these recommendations would help allow us move towards a more reasonable approach in lower risk disease.
REFERENCES:
Fifteen-Year Outcomes after Monitoring, Surgery, or Radiotherapy for Prostate Cancer
https://www.nejm.org/doi/full/10.1056/NEJMoa221412210-Year Outcomes after Monitoring, Surgery, or Radiotherapy for Localized Prostate Cancer
https://www.nejm.org/doi/full/10.1056/nejmoa1606220Patient-Reported Outcomes 12 Years after Localized Prostate Cancer Treatment
https://evidence.nejm.org/doi/10.1056/EVIDoa2300018