PPS and Protons!! The ROCR Exemptions...
Last week we discussed ROCR and a few things seem to draw most of the critiques of the plan - today we'll look at bit closer at these issues and beyond.
Sometimes Twitter is funny - often due to a level of truth. Good comedy comes from a perspective of truth. Here is my favorite summary post on the ROCR topic:
We are told that ROCR is our last hope for survival, a lone oasis in the Sahara of #radonc's future.
Yet we're also told it's politically impossible to include PCHs or protons because it'd piss off so many power players. Is this because ROCR is a mirage instead of an oasis? Is it a real oasis full of drinkable water, but the power players have so much San Pellegrino and Dom Perignon that drinking water is beneath them?
Or is it like Baron Harkonnen splashing a handful of water on the ground and telling us commoners to be grateful we have something to drink? @dschan02
And with that little zinger, today we will begin to look at critiques of the plan.
Last week’s article giving a broader context from my personal perspective:
PPS Excluded Facilities:
I start here because this one is more straightforward. I do think the ASTRO town hall initially offered a rather poor answer: (my summary) it is a big legislative effort so we can’t do that. When in fact, the ROCR proposal seems to me to be a really big legislative effort - from what I see the largest single specialty carve out from the traditional fee for service model - so that argument doesn’t fly far.
(I should note CMS has rolled out an entire - medicine wide initiative to move towards bundled payments for all services within the last few years LINK- we’ll get back to this briefly below).
But later in the “town hall”, they talked about the politics. And this to me was more on point: the question becomes, should our specialty tightly attach its goals to the removal of this other exception to the rule? And while it may an “idealistic answer” - is it politically the most appropriate path? And I think that answer is to me rather clear:
No.
Really quick: PPS-exempt Cancer Hospitals (hence PCH alternative language) get more reimbursement from CMS due to legislative acts - 11 cancer hospitals. I outlined them and the associated legislative pieces last week if interested).
In the PPS-exempt battle, we represent a minority of power and control. Singling it out in ways would pit us against 11 large powerful institutions and against, on some level, medical oncologists and radiologists and surgeons at those hospitals. And ultimately if and when it does go away, I personally think it will likely be within the context of CMS savings - not redistribution of the funds, but time will tell.
There is some pressure growing in the direction to have these exceptions be removed, even from within the Government Accountability Office (Payment Methods for Certain Cancer Hospitals Should Be Revised to Promote Efficiency). So do not loose hope and I wouldn’t say bury the issue completely, but I think to link it directly to our cause is unwise. And that is the real question from my perspective.
If you struggle to see this perspective (which I think I might have 5 years into my career), I’d encourage to talk and discuss the issue with people with a few decades of experience, high within organizational charts, or reach out to a mentor with board or chairman level experience and ask candid questions and try to listen for a different perspective. The blending of idealism, politics, and business is difficult to understand. A different beast contrary to much of what we need to accomplish in the clinic on a daily basis to deliver excellence in care - it is, in ways, directly opposed with the “day job” of medicine.
And so to me, I think True, True, Unrelated. (well kind of, but in our best interest to let it be a parallel track rather than fundamentally linked and that part I feel reasonably confident in).
Protons are Excluded (and other “New Tech Services”):
The larger issue for most: the exclusion for protons. This seems to have taken center stage in the debate. I think people rightfully come to these issues / decisions / compromises and see clear bias or, at a minimum, lack of equality in how protons seem to “escape” the legislative approach - now for a second time (think RO-APM).
As the analogy up top asks, if this is the magic pill, why won’t the proton centers swallow it?
And while I think those views are quite valid from certain perspectives, I’d just back up a moment and ask what is best for the field? Give me a moment as I try to explain - but I have listened / read hours of the this perspective and I think I “get it.” - I think.
Today, I’m going to just focus on context. I think there is a strong legal argument why protons would ultimately not be able to be included regardless due to the cost structure of protons compared to photons, but that is beyond the scope of today’s discussion. For those interested, THIS ARTICLE discusses that topic (see Comparative Effectiveness Research section or CER which even includes IMRT as an example case). It is well written and reasonably concise.
One perspective is an ideal approach and the other more nuanced and full of compromise. The later from a broader / longer timeline perspective that considers the capital investments for photons vs protons (and to a lesser degree MRI linacs) and then extends those conflicting views to the totality of our field. I tend to take the broader view / later view. One isn’t clearly right and one isn’t wrong - no one can predict the future.
As an example, I talk to Jordan Johnson occasionally and in places, we see things in a similar light, but often we don’t. He sees the world generally through an even broader photon dominated rural business perspective and I slant more holistic / idealistic often from a “protect the physician as the centerpiece of the solution” approach. Each perspective carries its own bias. In contrast, on this specific topic I guess I “swap sides” to the broader perspective landing more on the business side of the argument. I don’t pretend to believe one is right and one is wrong. Where / how you land on a topic is likely due directly to your past and current perspectives.
And including 100% of services does seem to be the more “perfect” / “ideal” answer. But here, I do think it is wise to step back and consider a broader context. Here is my perspective.
An intro point or two:
First off, what has been done, has been done. We can impact tomorrow. And today, we are trying to impact tomorrow working from a relative position of weakness.
Look at the match data as just one example or declining revenue or a number of metrics, which at a minimum, demonstrate weakness. And so, while we might align on the side of really disliking the initial models that allowed protons to prosper in growth without robust data, I think there are times when one must look in the mirror and perform some self-assessment. Here I think we need to consider the larger perspective of the field and acknowledge that the path we are on is at least quite dangerous for our field. And it is from that context that ROCR has been proposed in an attempt to change our course moving forward.
Secondly, proton and photon machines are factors different in costs. The facilities differ by a far greater factor in costs to the difference in payment factors by Medicare. Say protons reimburse about 2x for an episode of care via Medicare - treatment code is around $1200 vs $450 but total weighting is a bit less than 2. Ok, Emory, Maryland, New York - all of those are over $250M facilities. And as we have discussed in past articles, at current install / build pricing protons are generally NOT profitable today in a Medicare environment - not even in a PPS exempt Medicare environment. They require good contracts, great management, and likely some level of philanthropy.
In contrast, photon machines that can perform SBRT are available in the Oklahoma market for, basically, the cost to move them - a few hundred thousand gets you the facility, vault, and machine. Same in Arkansas. Yes, you can get a new tricked out for likely around $5-7M (guestimate) or so but you have options. Heck I think even the new Tomotherapy unit and the Halcion both offer new SBRT off the rack options closer to $3-4M (guestimate) while providing staff efficient platforms and relatively easy and quick installs. And therefore photons are still quite viable with >15-20 patients under beam (a bit more than a half day of patients). Maybe a single room proton facility at 40 patients can get towards viable depending on insurance mix but that really can’t happen outside of really unique circumstances and it requires an exponential level of work compared to a photon model to make a successful venture.
So to just say “take the pill”, to me as someone with about two decades in the business side of this field, is simply not practical.
Idealistic? Yes.
On point and so direct it hurts? Yes.
But practical in a business dominated US healthcare market? No.
(Quick aside: a recent editorial in our field, to me, perhaps implied that proton facilities might be imminently closing - I thought the language in that sentence was confusing / misleading at best. While I’ve stated here that proton facilities are generally struggling to reach viability, I don’t know of a single pending closure and I expect all of them to continue operations providing care to their patients. I’d refer interested parties to this Forbes Article from late 2021. As always, reach out or comment below - happy to edit / improve anything).
The Light in the Tunnel:
Remember today, the light in the tunnel is a hypofractionated train cruising at high speed towards your revenue center. ROCR attempts to create a framework to stop that train. And if we were to bundle all new tech, including MRI linacs and proton therapy, you begin to loose even more viability on a business proforma for those approaches. Today, these are already an uphill climb. Should we raise that barrier even higher and strengthen market forces that have already begun to significantly impact their viability? I don’t see that as the wise path.
If you doubt the struggles in these “advanced” areas, look at the ViewRay bankruptcy, or the number of rural radiation clinic closers or the number of proton centers that are struggling in this “new world” environment.
And protons will not be protected.
Here, I probably break from the masses with a different perspective. One I haven’t heard voiced aloud, but one I’m pretty sure is valid. As always, read and consider and you decide.
If you are CMS and you have been discussing models with ASTRO regarding payment options and ASTRO instead successfully deals with the congress to achieve a legislative win, what does the landscape look like? To me, from the CMS perspective, even without intent, your ability to impact change - your “dashboard” for radiation shrinks to 1/10th the scope it was. What before might not rise to the top will be clear and obvious.
So IF this would pass and possibly be implemented in 2026 or 2027, any proton growth or new technology growth would now jump off the global specialty dashboard for CMS - think replanning on the MRI Linac side which even today is garnering attention for the exponential growth rate it has. Remove the surrounding stability of the field at large and these types of items are in fact much easier to notice.
In fact, from the proton standpoint, I think IF ROCR gets done it is likely a significant pressure on the proton industry. Yes, if bundled and forced to accept photon payments tomorrow it would be even worse, but ROCR aims to first stabilize the photon world and from my perspective, then accelerates the downward pressures on protons (assuming no significant improvement in randomized data). And really that IS what the people who use this argument would like to see - more penalties on the proton side. In a very direct way, this will put protons on an island and therefore make their costs more visible. Today what can hide will not be hidden.
I’m guessing the people at ASTRO considered this different perspective - they understand the risks of the policy and realize that basically, if ROCR passed, you immediately then pivot and need to work on episode payments (or some other approach) for the last 10% pretty quickly. But I think they are balancing options and actively choosing stability for a broad cohort first - my guess.
It is often discussed that maybe the proton entities really drive the ship at ASTRO - that they command all the power. I think it is more balanced. Consider if the “powers that be” had opted to stabilize proton payments first with proton cost averaged episode rate model and left the photon side in a declining fee for service arrangement. I’m telling you, I can’t be the first to consider these implications.
So protons and MRI linacs won’t get a pass in my view. They will each continue to have the overlying pressure related to attempting to validate their cost / value proposition. To me, this model increases the scrutiny on these advanced technologies when compared to the current model because the CMS affectable pile shrinks.
And even since the development of ROCR (which I assume took a year or two), we now have a another example of a major capital investment issue - ViewRay. The first is the clear inability for many proton centers to make debt service payments and now ViewRay and to a lesser degree the third with the GenesisCare bankruptcy. To me, the more people argue for protons and MRiLinacs to be universally bundles, the more likely ViewRay never recovers. IF, today, one were to bundle all payments even at say $500 more per episode for their inclusion, there would be even less reason to purchase that company. I’ve peered into the rabbit hole - there are real reasons it trades today under 0.02 cents with no residual market cap (from well over $1B) - recent dockets discuss utilities - literally keeping the lights on. The very basics are at risk during Chapter 11 filings. (I remain optimistic here with bids due in September but risk is real).
Heck bundle all payments and take out new technology as an opportunity and I’m not sure why Varian would continue to iterate and improve technology over accelerating the efficiency, throughput, via a “robust enough” technology path. So there are ideal answers in idealistic worlds and then there are compromises that need to be made to help balance out our field for future strength.
Perhaps that isn’t enough “punishment” for some for less proven technology, but I think it is quite different from the free pass that I think some people might think this delivers. And for those reasons, if you initially voiced non-support for ROCR due to the technology exemptions, I think you might reconsider - I think it actually accomplishes much of what you want to see - increased attention and visibility of the small segment of our field that is relatively high cost and technology driven that needs, as I have argued, to continue to prove value via good solid science.
As I say:
Until I have x-ray vision and shoot radiation out of my fingertips, I rely on technology.
Remember, most of the technology that we use in the clinic was rolled out prior to clear prospective clinical validation of benefit. Based on principles - we moved from tape to masks. We added IGRT options. IMRT was largely adopted prior to validation of benefit. 6D tables etc. etc. Tools to help us put dose where we need it and not where we don’t. Whether that fact of history is good or bad, or good up to a dollar figure and then bad - that is a complex issue. But leaving an opportunity for that general process to continue into the future I believe is wise as we try to compete in a national competitive marketplace.
Is Action Truly Required:
This… this is the real question. Within minutes of my post last week it was summarized well in the following comment.
Mark great article. But nothing you write makes the case for ROCR. Spreadsheet analysis shows it to be a net loser. And once we are 'a bag of chemo' our specialty will suffer even more as it becomes easier to cut away at one code. Congress can't save us but dramatic reduction in the workforce via training could. But that won't happen.. the outlook is grim.. (Jay)
And this critique is the hardest to address. Just because you *think* you see an outcome on the horizon doesn’t mean drastic action is required. Should one be measured and essentially dig in and fight like stink to remain near “status quo” or jump ship from the current path and attempt to adapt to “pre-emptively” maybe avoiding what we think might happen.
Here, even though I really have no inside information, I presume we’ve been attempting the former for the past decade, on the ground and in the trenches, and yet, the train keeps hurling down the track. And so now, they are opting to pivot. They have decades of experience on the path attempting to do the “dirty work” and yet, are opting to change course. I think that perspective therefore carries real value.
To me, discussion around this point: stay the course or move towards a case rate approach is the primary discussion that our field should have. How each can / will affect our workforce issues and allow us to stabilize our footprint in providing value for oncology. I think the more perspectives we hear and consider, the better prepared we will be to address future hurdles.
So is this all about money and funding? And is total revenue into the field really a good way to define benefit for ASTRO members at large, which is labeled as a physician led organization?
For me, it is not just about the money. Money certainly is a central component of the decision but it is far more complex. Today I see our field as divergent in too many places - whether it is on protons or whether hypofractionation is great or dangerous. And as I’ve argued we need the general pendulum to swing back towards the center. Due to our small field, we need a more unified voice than we often present publicly. And to me, IF we were to see a case rate approach, then I think there is opportunity for field to be more united.
Does total revenue even matter to physicians? Many might argue that employed physicians who are paid off of wRVUs on the professional component are not impacted, but in my experience, that is a rather limited view. It is true that the majority will be unaffected on a pure dollar / contract evaluation. To me a large portion of medical professionals, on some level, opted for medicine as a way to avoid business. So the vast majority will take what is offered with little broader attempt to quantify their value - happy with (my words) a generous payment for services while able to impact the lives of patients via the clinic or lab.
But the money into and out of the specialty affects the margins - the 25% or so who do assess value and that will impacts the 75th percentile, the upper tiers and even the mean incomes. And for all of us, the technical revenue supports your staff and technology - computers, software, number of therapists, nurses, physics coverage and pre-authorization assistance. The two components are intimately linked and when 80% (and growing) of the funding is on the technical side, the technical component dominates how your clinic operates.
Real Risks with Altering the Course:
But there are absolutely real risks. Any government transition on this size and scope will cause chaos for months in a perfect scenario - as different payment systems and different approaches must be blended and that is why I voice my thoughts as one opinion.
There are risks of allowing a single code change to have far greater impact. There is massive disruption of process between Medicare and potentially Medicare Advantage plans and private insurance. There are coding differences and upgrades to computer billing software that would be required. Systems on this scale simply WILL NOT transition without major impact (a year or two) to many of the smaller practices in the US. And there is a question of priorities: is this the right place to expend most of the effort? If one were to choose to stay on the current path, we would have additional resources to place in different areas - say promotion of NCCN guideline support, or integrating systemic therapies into our training programs, streamlining accreditation, or addressing workforce issues. There are, after all, a multitude of options in which to move forward.
But, at the same moment, status quo payments are off the table - remove that thought. Fee for service is a pathway to annual decreases in reimbursement. Hypofractionation / omission will continue. AI/automation create risk for critical code downward re-evaluations. And CMS, at some point, has stated its goal to carry all of medicine over a case rate cliff on their terms. Some of these may never happen, but some are guaranteed.
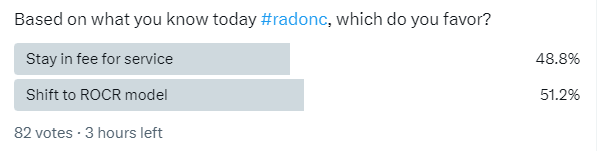
So you end up with a simple question. ASTRO has announced ROCR and attempted to support its rationale for this major shift with a webinar. I don’t know how well this cohort would match a larger, broader section of ASTRO members but… wow.
To me, ASTRO needs to have this be a clear, repeatable, majority. Again, I like and support the concept of ROCR, but if it is me driving the ship and I can’t get this to 67% or ideally closer to 75%-80% support, then it is likely not the best path. From here, ROCR will change. It will weaken and shift during the legislative process - it will contain more burdens in the future than it contains today. This new path is filled with unknowns and even if passed, the transition will be difficult. You need strong support from in my opinion to begin such a massive change of direction. And while I support it, I believe it needs to be rather broad consensus opinion that drives us forward.
In Closing:
Today, I’ll end with this:
As radiation oncologist - we provide value care. Slice it anyway you wish. Talk about the dollar / costs benefits of technology - whether that is MRI or protons or other drivers of spending increases like IGRT - we provide massive value across a vast spectrum of cancer patients. That is one of the basic principles that I try to demonstrate on this Substack.
In fact, one might argue that our own field’s push to be more and more efficient and cost effective in an otherwise terribly expensive/wasteful marketplace is the very reason we REQUIRE some more significant moves and creative approaches to ensure our future. I’m not sure I can point to another specialty that has done so much work on an idealistic front in order to attempt to prioritize patient quality of life, almost directly, shrinking our seat at the oncology care table.
But due to the speed of change, it is prudent to build a bridge from the past to the future. And ultimately that is where I think I see this approach. It is ASTRO attempting to stabilize the field so that the physicians can keep pushing for better within today’s environment.
Not perfect - nothing is. Full of compromise - has to be. Perhaps even too late - maybe. But a shift towards the correct direction - I believe so.
Just one perspective.
Enjoy the week! Looking ahead - three positive radiation trial results: one in lung cancer and two with protons: one in hepatocellular cancer and one in prostate that I look forward to diving into. Thanks for following along as we search for better.
Edit: repaired two words, added an “a” and removed an “ly”.







Nice discussion as always. Would’ve liked to hear from you what points a chairman or board-experienced MD would make re: PPS exemption. Also, my understanding of the current Medicare dilemma for rad onc is the budget neutrality forces steep cuts to expensive tech-driven fields in order to raise reimbursement to cognitive specialties. Is that not correct? If it is, then I respectfully disagree with your hypothesis that ROCR would lead Medicare to specifically punish proton therapy. It seems that the usual budget ratchet would continue the same course as it always has. I.e. the statutory cuts would continue to come, but proton owners presumably accept that.