Market trends: A Rebuttal
A recent article made my blood boil. We'll look deeper and see if my gut was right or wrong.
Financial toxicity is an important topic. It impacts the lives of cancer patients and it affects the very foundation of our national budget and, more importantly, the financial and mental health of our patients. It is a very reasonable and appropriate area of healthcare to explore. Sincerely, kudos to those who attempt to work in this difficult and complex space.
That said, I’ve worked in this space for nearly two decades - on the ground, front line work. Part of my goal in moving to part-time is to attempt to broaden my impact in this space. So when I read things on this topic that I think miss the mark, it is frustrating. But really, the question then becomes, was my 2 minute impression correct or off base. And to figure that out takes quite a bit of time and self-assessment.
Today, nearly two months later, we’ll walk through my perspective and why I still think I was right.
Our Starting Point:
This recent article looked at practice trends and made a clear decision to parse the US into “hospitals” and “freestanding” centers. Here are some of the pertinent headline statements from this analysis.
Evidence supports the value of shorter, similarly efficacious, and potentially more cost-effective hypofractionated radiotherapy (RT) regimens in many clinical scenarios for breast cancer (BC) and prostate cancer (PC).
Median total spending for SCRT(short course) regimens among BC episodes was $9,418 (IQR, $7,966-$10,982) vs. $13,601 (IQR, $11,814-$15,499) for LCRT(long course). Among PC episodes, median total spending was $6,924 (IQR, $4,509-$12,905) for SBRT, $18,768 (IQR, $15,421-$20,740) for moderate hypofractionation, and $27,319 (IQR, $25,446-$29,421) for LCRT. On logistic regression, receipt of SCRT was associated with older age among both BC and PC episodes, as well as treatment at hospital-affiliated over freestanding sites (p<0.001 for all).
CONCLUSIONS:
In this evaluation of BC and PC RT episodes from 2015-2019, we found that shorter-course RT resulted in lower costs vs. longer-course RT. SCRT was also more common in hospital-affiliated sites.
And the first sentence of the discussion reads:
In this analysis of episode-based CMS data from 2015-2019, we found that utilization of SCRT regimens resulted in decreased Medicare spending for both BC and PC episodes, and that receipt of SCRT was associated with older age and treatment at a hospital-affiliated center.
My Caveat: Short course treatments are lower cost. In a fee for service payment structure, shorter courses are less costly. Hospital sites have moved to short course treatments quicker than freestanding sites. But one MUST keep short course utilization separate from cost of care based on site of service - they are different items and can be dominated by other factors beyond the scope of the article which, instead, implies a direct association.
Framing Today’s Discussion:
What I believe is quite incorrect is the direct linkage of 1) short course treatment to 2) cost to 3) hospital setting. That same message is mirrored in the abstract and discussion. If you just read the headlines, you likely come away with an incorrect assumption - that hospital treatments are less costly.
Today, we’ll show that their data illustrates that hospitals are, in fact, more costly despite fewer fractions - quite different from the headlines and the discussion.
Further, I believe my argument is completely consistent with broad context in healthcare. Re-read their conclusions and statements. Then consider the following statement which I believe is correct:
If all treatment moved to a freestanding setting - using their data - total cost of care would decrease by $16M.
You see, breast cancer was cheaper to be treated in the hospital, with potential savings of $19.5M. But prostate cancer was cheaper to be treated in the freestanding setting with potential system savings of $39.4M. A net “potential” win in favor of freestanding facilities of $19.9M over the study duration. Yet, is any of this within the headlines or in the abstract - nope.
Now, we’ll look at my perspective and consider broader context that should have been acknowledged and, yes, math.
My Editorial Beginning Comments:
Why does this bother me so? Because I see it as so very myopic; lacking self-awareness. It then was openly stamped by our professional organization at a time when we are seeking to fundamentally change how we bill for Medicare to an episode based model.
And it happens all the time with protons. People who are reimbursed for IMRT at higher rates than freestanding facilities are reimbursed for protons, write articles condemning the “costs of protons”. This is the same issue - just, for some reason, choosing to create a division between hospital and freestanding facilities.
If you’ve read things here before, hopefully you appreciate that one of my main goals is to argue for the tremendous value we provide - I work hard not to pit one group vs. another, but rather develop a holistic and unified view of our specialty. I enjoy those, far more than writing this piece, but each are important for us to move forward.
Today I’d like to present additional context that this article does not address. The scale and scope of the dollars I will present dwarf the differences found in the paper and therefore renders the publication superfluous and damaging to our goal of unifying our specialty on an important topic of cost control, future payments, and financial toxicity. Further, based on the publication, their own data argues against their chosen path to link cost to different sites of service. The hope is: you leave with more context related to this issue.
Author Affiliations:
To me, the authorship is problematic for this type of specific work. There are 12 authors, one of whom represents the specialty society leaving 11 physicians. 8 of 11 work within institutions that are PPS-Exempt. Four (of 11 total) separate PPS-Exempt institutions are represented. The three remaining work in highly prestigious US institutions.
There is no freestanding representation. There is no representation of small academic programs that compete on a more level playing field with freestanding facilities. There is no representation from anything in primarily rural or even within the center of America.
I think this degree of unbalance in the authorship likely limits the real-life experiences and perspectives available. To me, that is largest risk in such a non-diversified authorship.
For open context, I’m affiliated with a proton center. I’m an hourly consultant - practice of one - flat daily rate regardless of work or RVU or revenue to the center. I have treatment options available for both protons and photons. I have access to machines within a metro region and in a more rural setting. Purposefully as independent to site, modality, and fractionation as I can get. Prior to this I worked in a single room satellite facility in Arkansas, serving towns like North Little Rock, Jacksonville, and Ward again within a freestanding facility arrangement. I trained at MD Anderson. It is nearly the opposite end of the spectrum - a large PPS-Exempt hospital setting. I consider myself to have reasonable variety in my 25+ years within the field. And I fully acknowledge I have my own biases that I brought to my reading of the paper.
Does Location Have a Known Impact on Cost:
Absolutely. (REF)
The lowest cost state represented in the article authorship is Florida. #11. Six of the 12 authors reside in #1 or #2. For context, I have spent the entirety of my practicing career in #50 or #44.
As shown, Medicare FFS rates do change some from about 0.85 to 1.2 from low to high - a factor of about 40%. In contrast, for commercial contracts (that now include Medicare Advantage options), the difference is far greater from 1.5x - 4x Medicare approaching ~250%. So any Medicare analysis will be very muted relative to actual healthcare dollars.
What type of Impact does PPS-Exempt have?
Briefly Define PPS-Exempt (my words): PPS-Exempt hospitals have been granted an exception to Medicare payment rates - they receive additional payments per passed legislation. PPS-Exempt is then abbreviated PCH. So the two versions you will see are: PCH or PPS hospitals.
This is the good older reference document. (REF) It is from 2012. In this United States Government Accountability Office Report, PPS-Exempt hospitals, on average increase costs per inpatient discharge by 42.3% as of 2012.
The Government Accountability Report reads:
However, the health status of Medicare beneficiaries with cancer who were treated at PCHs and PPS teaching hospitals was not markedly different.
And it is titled:
Payment Methods for Certain Cancer Hospitals Should Be Revised to Promote Efficiency
Finally, they recommend:
What GAO Recommends:
Congress should consider requiring Medicare to pay PCHs as it pays PPS teaching hospitals, or provide the Secretary of Health and Human Services (HHS) with the authority to otherwise modify how Medicare pays PCHs. In doing so, Congress should provide that all forgone outpatient payments be returned to the Trust Fund.
So my summary is - at a minimum, these institutions carry significant legal and structural power within our healthcare system - enough to be granted an exception to basic payment rules of Medicare. They are granted additional compensation for services that the Government Accountability Office finds ultimately delivering health status that was “not markedly different”.
And yet, it is not stopping. Just so you understand the power these institutions wield, here are the estimated payment adjustments in OPPS Payments for 2024 due to Payment Adjustment: Final OPPS rule.
H. Lee Moffit: 25.0% (up from 9%) above
Sylvester Miami: 41.9% (up from 20%)
Dana-Farber: 43.1% (up from 8%)
Memorial Sloan-Kettering: 58.1% (up from 20%)
(these are government estimations for additional payments to these hospitals relative to local hospital rates - so local market “bumps” in payments for same services all rising relative to 2015).
In summary, while the rest of us fight off payment cuts, each hospital above has increased its pay gap granted via special legislative exception relative to 12 years ago.
Price Transparency:
Further, I’ll refer to a price transparency table related to one of the affiliated institutions that does NOT enjoy PCH status, just to demonstrate the power large institutions have on many levels.
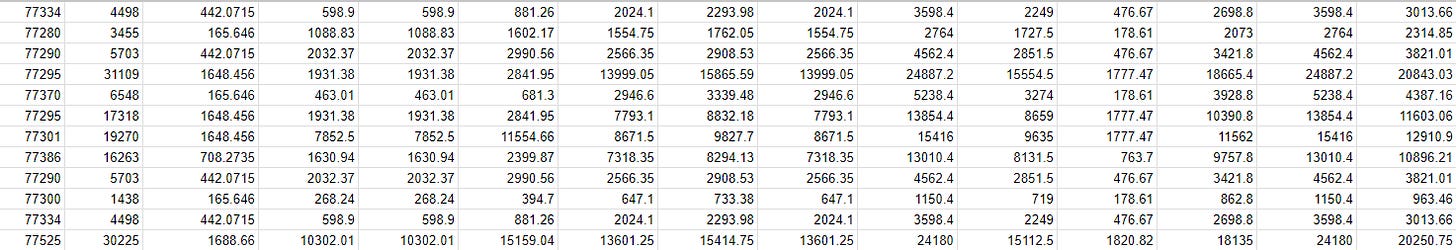
I know this table appears very small. I know I kept off the headers and I purposefully removed the name of codes and just left the technical codes. I just want to make points, not be a reference document.
Column 1 is the CPT, column 2 is charge, column 3 is discounted cash and then you have 12 separate individual negotiated payer contracts.
I understand that making it harder to read hurts my argument in ways, but I respect the institution that openly publishes this information with payers and values. Its all findable via an internet search if you know where to look, but I think if you want it - you need to go track it down. It is all valid / current and public data per week 1 of December 2023.
Here are the highlights? / lowlights? of the table above.
$15k per fraction for protons. Paid. Billed at $30k per fraction. A complex device - billed out at $4500 and PAID at more than $2000 in eight instances in the small section above (as high as $3600 per device). Just for reference according to CMS public records, in Arkansas the billable amount for my affiliated non-profit (was in a consulting role there as well) was $486 and my average Medicare payment was $93. Dang… Any and every freestanding center in the US would kill to have anything near these reimbursed rates.
Wait - this is apples to oranges. Correct, yes it is.
Completely agree. One is Medicare (my rate of $93) and one is private insurance for a hospital (average of the 13 is $1850).
But you now have context. Go to the regional graph above and pick the mid-point nationally. Nationally you can see that private insurance contracts pay about 2.5x Medicare. In Arkansas that was a really strong rate. In fact, billing companies will often suggest setting pricing about 5x Medicare - a discussion for a different day, but pay for a consultant and that is about the number they recommend (at least where I’ve practiced).
Example: Look at my data - $486 is the charge: basically 5x payment rate. And across the state of Arkansas, the review above placed private insurance reimbursement at about 1.5x Medicare. We got closer to 2x-2.5x if I recall correctly. We worked hard in this area.
But here, the difference is 20x. That is the power that these large institutions have in Medicare Advantage and private insurance negotiations. Meanwhile, traditional Medicare is an ever shrinking portion of the revenue stream. And per that same graphic, you can see that payments for Medicare do in fact vary by region - not near as much, but there is a cost of living adjustment in the calculation and payments do vary.
Why not show Apples to Apples?
Because, by far, the most accessible data is Medicare data. The other data is much less freely available and really far harder to access. So the authors did what nearly everyone will do - they examine the portion that is easy to evaluate. But that doesn’t make the other go away and everyone working on “the business of medicine” should recognize this openly.
Presentation Accuracy:
Unfortunately, the article also has clear errors. I’ll give just 3 examples demonstrating how poor the data appears from afar.
Table 1 is too large to copy here. For prostate cancer:
There are 27 SBRT “long course prostate cancer treatments” - so 27 times, the database is saying they billed SBRT while giving 30 or more treatments - clearly wrong.
The IMRT utilization rate for long course prostate treatment was 0.37% (328/88259). For reference, an RO-APM document put that same number for years within this exact study timeline at 66%. Less than 1% is simply wrong.
And then attention to detail: First from the text of the results:
Of 143,729 BC episodes, 80,106 (55.73%) were SCRT regimens and 63,623 (44.27%) were LCRT
But Table 1 then shows:
SCRT as 63,623 events (44.27) with LCRT at 80,106 events (55.73).
Yep, exactly the opposite. One is correct and one is wrong. It is a clear copy / paste error. I believe the table is correct. I believe the text in the Result Section is the error. My rationale: if you look at the graph of short vs. long, they cross later in the dataset. Therefore assuming relatively similar numbers of patients for each year, the cumulative result should favor more in the long course. Note: that the trend “today” is now the opposite with the graph “reversing” in 2018. Regardless, another clear error.
My hope is that the data submitted was good but somehow in a push to HTML and out the door, that things got messed up and then they were published in this current state with multiple clear errors.
On this note, most of my comparative math comes from two statements regarding breast cancer treatment costs and prostate cancer treatment costs - if these are also incorrect, my math would be wrong.
Do I believe the any of the findings?
In principle, yes. Submit less charges in a fee for service setting and they will, in fact, send you less money. 100% agree. So yes, short course treatment will pay less.
Have hospitals have been quicker to hypofractionate? Yes. But….
I believe there are two additional reasons that need to be discussed that were not mentioned. Large hospitals and academic centers have two important reason to hypofractionate faster.
It is a marketing tool to pull business away from outlying competitors to the big hospital. No one “travels” to North Little Rock for treatment, but people travel to proton centers and big hospitals so it behooves them to shorten treatments from a “market capture” perspective. Far more than the place within 10 minutes of the patients home.
Academics have to publish - and in large volumes. You can’t publish the same old stuff over and over. You have to innovate and that is what they are doing - no fault. But a main academic narrative of the last decade within radiation has been towards shorter course of treatment. This, now blended with marketing reasons, is part of this shift.
Do I believe the hospital institutions are really looking to drive costs lower in a more earnest and honorable manner than those working out in a freestanding center? An emphatic no. Or because those physicians or programs are just better and more knowledgeable? Another emphatic no. Rather, each setting is simply competing within the market.
An Odd ROCR Link:
Finally, there is a paragraph that links this work to ROCR. It starts with this:
Moreover, contrasting radiation from immunotherapy, which account for nearly 84% of the observed overall increase in Medicare outpatient cancer care spending, hypofractionated regimens have consistently demonstrated cost-effectiveness in numerous clinical settings.
This bears repeating:
contrasting radiation from immunotherapy, which account for nearly 84% of the observed overall increase in Medicare outpatient cancer care spending
That is such an important point, but it is almost buried in the text of the article. What an amazing statement. It speaks to a common theme on this site:
Radiation Oncology represents tremendous value!
I believe we must be unified in our arguments to even compete with pharma. We are likely outspent 100x by pharma, and yet the article instead chooses to divide our specialty into parts and evaluate trends while ignoring so much broad context - at least, that is very much how it landed to me.
The article continues giving this “statement of fact”:
Indeed, integrated across all beneficiaries, the ROCR bundled payment program is estimated to save more than $200 million over the next five years
But here is the rub. This is a scientific article. The data in the article pretty directly addresses this “statement of fact” then referenced in the discussion. And if my offline spreadsheet math is correct, this very publication argues strongly that this proposed costs savings is incorrect.
I will not post my math directly here as it is not advantageous to our specialty but it is straightforward and quite striking. It should be a simple 15 minute exercise. (my goal is not to be a reference to fight against our own value). My math shows that this paper documents that even relative to CMS spending four years ago, ROCR represents additional costs to the government if passed. (Simply, long course percentages would have to increase compared to 2019 to reach ROCR payment levels. The reality, however, is hypofractionation is more common today than 4 years ago as we all know).
Whether this is “good news” or “bad news” depends on perspective I guess.
If I had had input to the paper, I would have suggested the following: this statement regarding ROCR should have been moved to the introduction as part of the thesis for the paper and then assessed based on the data. I believe the data shows it to be false. Either that, or just leave it out. Are we a science based article or an opinion article? Was the intent to evaluate or to persuade?
What could have been done differently.
My main points would have been to integrate more diversity into the authorship - to broaden the perspectives. Secondly, the database should have been more thoroughly cleaned and the basics of Table 1 (the central piece of data) should have undergone stronger QA - table 1 just can’t afford to have common sense errors of 0.37% IMRT for long course prostate cancer for this time period. Third, if this is going to attempt to integrate a political approach to the re-structuring of our billing, I believe it should have taken a data driven approach to validate the basics of the proposal or refuted that reference - clearly separating science from editorial. And forth, if you are going to delve into these topic, it is imperative that other system complexities are, at a minimum, described or stated within the limitations section - broad context is critical.
Below is the entirety of the study limitation section. I do think it speaks to the type of weaknesses inherent in this type of data. I think that is reiterated by the errors in Table 1. Further, notice no mention of “region”, or “PPS status”, or the blurred line that exists between “hospital” and “freestanding” (it is far less clear than nearly everyone would believe). Even “Protons” are excluded yet nearly all reside in hospitals and often carry 6 figure costs for most “hospital” settings:
Limitations of this study include its retrospective nature, the lack of available clinical variables, inability to discern the treatment intent and exact dosage of radiation received, and the limited number of years included in the analysis. There was also no distinction made between metastatic or localized episodes in the dataset, which may have skewed the sample towards shorter courses of radiation. Moreover, we were unable to remove all palliative episodes from the analysis because certain radiation modalities were not included as data elements in the file, such as three-dimensional conformal radiation. Nonetheless, by excluding patients with 90-day mortality as surrogates for aggressive disease, we were able to assume similar rates of palliative radiation across both analytic cohorts and mitigate misattribution. Ultimately, more research is warranted to better understand the usage, cost-effectiveness, and structural challenges of implementing SCRT in other disease sites.
In the end, some of the ideas are likely true, but it is far from a complete vision of the various factors for our field. Billing and financial realities are far more complex than simply hospital vs. freestanding, and yet, with little mention of so many important other factors, that is where this article choose to go, supported by our specialty society.
And it leads directly to this… a really high cost, PPS-Exempt center basically running an ad talking about their value using this study as their data for their value. Again, the implication of the post / ad is quite different if you have basic context of the issues we addressed above.
Read that again.
“shorter-course radiation resulted in lower costs and was more common in hospital-affiliated sites.”
It mirrors the words of the authors. Here is the first sentence of the discussion:
In this analysis of episode-based CMS data from 2015-2019, we found that utilization of SCRT regimens resulted in decreased Medicare spending for both BC and PC episodes, and that receipt of SCRT was associated with older age and treatment at a hospital-affiliated center.
But the data - directly from the results section is more nuanced:
Prostate cancer… increased among those that were treated at hospital-affiliated versus freestanding sites (adjusted β: $644.51 [$549.90 to $739.12], p<0.001).
Breast cancer… decreased among those treated at hospital-affiliated versus freestanding sites (adjusted β: –$416.63 [–$476.39 to –$356.86], p<0.001).
Which leads us to Math:
We’ll start with a simple approach.
Scenario 1:
Each setting was shown to be advantageous. Freestanding centers treated prostate cancer with less costs and hospitals treated breast cancer with lower costs.
In our first scenario, we’ll simply move all breast cancers to hospital settings and all prostate cancers to freestanding to look at the relative difference in healthcare expenditure.
Breast cancer potential savings (18k + 29k pts) *$416 (relative cost improvement):
$19,542,863
Prostate cancer potential savings (18k + 41k pts) *$664
$39,414,082
Total cost savings “opportunity” via this simple look favors a shift to freestanding facilities by $19M.
Scenario 2:
The next approach, where the math gets one more step complicated is simply to assume that there is no freestanding option - calculate relative gains and losses and then compare that number to the same approach assuming no hospital option.
This work is shown within the referenced spreadsheet (below).
This leads to difference between these two scenarios of $16M, again favoring a freestanding facility only approach.
Scenario 3:
Finally, you can consider trend lines and assume that at some point in the future, this difference will equilibrate around some “ideal” short course usage level. Say 20% long-term need to have long-course treatment.
This clearly has assumptions but the rate of change is likely near maximum today. There is a 10% gap in breast and a 25% gap in prostate. I think it is reasonable to consider a long-term ramp towards an ideal. Historically, there has been a gap between hospital settings and freestanding facilities of say 5%-10% (currently wider in prostate I think due to the “newness” of the data). We’ll assume a reversion towards a mean of 7.5 for both - hospitals remaining more aggressive.
There will likely always be some gap, but as you approach a 80/20 split, here are the numbers:
This scenario lands in favor of freestanding facilities saving $30M over a 5 year period relative to hospital settings.
Per episode, this type of trend line results in a simple calc of excess spending per hospital episode of care of ~$600 - still assuming hospitals delivering shorter courses of treatment. If you assume no difference in fractions, the episode reimbursement is ~$950 more costly in a hospital setting. Finally using this approach, one can determine that the gap between short and long course treatment approaches has to be in excess of 20% to reach approximate equivalent costs per episode.
(REF to fixed spreadsheet - shows all math. If I missed something, please comment or reach out).
Note just how different this perspective is from the Abstract and the Discussion from the paper. They are literally opposite in findings.
Finally with any math, I have always backed up and looked for context - does my spreadsheet work make sense? And I think it does. Beyond region, PPS-exempt, hospitals literally receive more government funding per CPT code.
Site Neutrality - a known imbalance:
Today, hospitals are reimbursed more for services. The history of this difference is beyond our scope, but this is a known imbalance. The argument to balance payments and remove this extra payment for the hospital side is called “site neutrality” - ie equal pay regardless of site of service.
“Site Neutrality” is opposed by the American Hospital Association (ref):
The AHA strongly opposes site-neutral payment cuts…
Here is a quick summary of the scope of this issue:
The Medicare Patient Access to Cancer Treatment (MPACT) Act (H.R. 4473) would create site-neutral payment cuts to services related to cancer diagnosis and treatment at offcampus HOPDs beginning in 2025. This would result in a cut to hospitals of $11.8 billion over 10 years.
As you know may or may not understand, ROCR achieves site neutrality via an episode based model. Inside of the ROCR model, “site neutrality” lies within a “black box” of an episode based model. This data, however, does allow one to estimate Site Neutrality impacts for our specialty, removing it from a “black box”:
My estimates are: Site Neutrality impact for Radiation Oncology:
Freestanding see a bump of $330.54 per prostate/breast case on average.
Hospital cut of $215.53 per prostate/breast case on average.
(my calc - completely from the data they presented. Simply: assume trend lines meet so gap goes to 0%. This give excess costs due hospital care. Divide by number of total cases. My ESTIMATE - assumes site neutrality impact represents ~66% of difference with others being regional effects and PPS-exempt effects).
Summary:
I spent a few weeks on this rebuttal. I feel pretty confident that my assessment is more consistent with broad context of reality than the original paper. My numbers align with known compensation differences based on:
Region
Site of Service
PPS-Exempt status
This data shows hospitals are more costly DESPITE less fractions.
Unfortunately, I think this paper ultimately misses that mark and leads to assumptions that can be 180 degrees away from reality.
We represent value. We are quickly moving towards shorter approaches that create more value. We need to continue to work on paths to improve outcomes. Each and every day we are gaining value relative to pharma due to our efforts.
Just a thought, but instead of dividing our field up into hospitals and free-standing, here is a post by a leader in our field from earlier in the year (referencing a different study but similar area of work) that reflects far more balance on the issue of hypofractionation.
I’ll close with that. If the article had taken a similar stance, it would have been fine. But it didn’t. I don’t like writing rebuttals, but this one needed more context.
Special thanks to Dr. Jason Beckta MD PhD - due to the divergence of this editorial to the original article, I did ask for a good peer review of this rebuttal prior to “publication”.
Out of the Basement Podcast (top link at this offsite link) - can find on Spotify, Apple and Google Podcast platforms. Like the content here, it dives deep into odd and strange regions of the world of radiation oncology - hence a favorite of mine and why you will sometimes see a few of his thoughts creep into my writing.
If you learned something today, or might think about things differently, please like or share the article. It really does help. Thanks in advance for your support. If I missed, please reach out or comment.








We have to remember health care is the biggest price fixing scheme in America. Someone or group is coming up with these numbers. Why do I make as much as I do as a radiation oncologist compared to a PCP? Some group in DC negotiatiated my pay.
However I did enjoy the article and agree. However there are way more variables. One is the incentive to have physicians-scientists, 2 to cover the cost of the uninsured and underinsured 3 pay for research 4 have radiation oncology departments support other departments in the hospital etc