Esophageal Cancer Awareness Month: The argument for Proton Therapy (ADVOCACY SERIES)
Randomized Prospective Data supports Proton Therapy over IMRT for the treatment of Esophageal Cancer - especially if you are a potential surgical candidate.
www.protons101.com
Home to the musings of a radiation oncologist - with a slant on protons and dose and optimizing cancer outcomes.
Today is more of a patient advocacy post. If you are not aware, Esophageal Cancer Awareness month ends today.
My recommendations today are outside of what is standardly recommended. This data that was published in March of 2020 has largely been dismissed in my view, but it is a prospective, randomized data coin flipping patients between IMRT and proton therapy (mostly older passive scanning proton therapy) and it shows dramatically less toxicity for the patients treated with proton therapy.
So today, we’ll roll through the trial and discuss why I believe that an esophageal cancer diagnosis is one that I would recommend for my friends and family to consider travel - even out of state - for proton therapy - especially if I thought surgery was a treatment option.
On a reading difficulty level, this is between medical literature and patient piece - hopefully it bridges that gap successfully.
An insurance caveat: The US healthcare system is amazing complex and insurance may or may not support proton therapy despite the data we will review. If you are considering travelling, make some phone calls to the center and discuss insurance and your financial situation. With any serious cancer diagnosis, time to start treatment needs to be minimized.
Esophageal Randomized Phase IIB trial: Protons vs. Photons
Trial Summary:
Protons have a dosimetric advantage over IMRT (fancy computer driven traditional photon radiation) - ie they put more radiation in the target volume and less other places due to the physical properties of the beam - they are not perfect or magical, but they generally decrease the radiation dose outside the target volume by about 50% compared to the very best IMRT plan. So the basic question becomes:
Can this improve outcomes by reducing toxicity in patients with esophageal cancer treated with concurrent chemotherapy radiation (about half of whom went on to surgery)? (ref 1)
The two primary outcome metrics for this trial were total toxicity burden (TTB) and progression free survival (PFS). TTB is a created cumulative toxicity scale created at MD Anderson. The goal is reasonable: measure cumulative toxicity over time between two treatments, but it is not a common well-known outcome metric. And although elegant and seemingly well designed, I believe it ends up being a weakness and argument against the trial outcome as we will discuss.
In the trial, both approaches (IMRT and protons) deliver the same dose. So the expectation was to see equivalent cancer control with less toxicity in the proton group. The only real path for protons to “win” on cancer outcomes would be for the IMRT toxicity to be so much worse that we see many more additional treatment deaths in the IMRT arm - the trial was performed at MD Anderson and realistically with experienced teams - this option was nearly zero - so this trial is best viewed simply as a toxicity trial.
So here, the technology advantage is not utilized to increase dose or reduce margins, but rather simply to attempt to demonstrate a reduction in toxicity within a well established standard of care therapy where treatment toxicity is high.
Patient Characteristics:
145 assigned - 107 evaluable. Arms seem well balanced - an extensive Table 1 of patient characteristics shows only Zubrod performance status was different in favor of the IMRT patients (total, IMRT, proton arms with p=0.02 - or stated differently, the proton patients were a bit sicker before any treatment).

Quickly addressing the drop from 145 randomized to 107 evaluated. Main issues were insurance denial on the proton arm and requested proton in the IMRT arm as shown below (« see, here is the insurance issue showing up). Not ideal but data openly presented and expected in any proton therapy trial today and again, an extensive Table 1 shows well balanced arms.

RESULTS:
Dosimetry Differences:
Pretty simple here. Tumor coverage is as good with protons while dose to normal structures is less with protons.
The table basically becomes a restatement of what protons can provide over IMRT. Two examples: look at total lung v20 - the volume of lung treated to about 40% of the prescribed tumor dose - 13.6% for IMRT vs. 8.4% for Proton therapy. Or heart - mean dose of 19.8 with IMRT falls to 11.3 with proton therapy (there is a really large portion of our radiation literature that links heart dose to major acute cardiac events - ie heart attacks - higher mean dose, more cardiac toxicity - in this trial protons delivered 40% less dose to the heart).

Note: newer proton machines today should amplify the dosimetry differences - 80% of patients in this trial were treated with older passive scanning approaches.
Outcomes:
Total toxicity was markedly reduced in the proton therapy arm. This is even with 80% of the proton plans being delivered with passive scanning techniques. IMRT had 2.3 times the total toxicity score of PBT. In the ~50% of patients undergoing surgery, post-operative complication scores were 7.6 times greater in the IMRT arm.
Here is the Total Toxicity Burden list with weightings - this is stuff, that you do not want (stroke, heart attack, fluid on lungs, leak of fluids where they sewed things back together etc. etc). To find this, you have to cross reference the document originally describing the Total Toxicity Burden methodology which can be found here (ref 2).

The primary outcome visuals for the paper are shown below. It is both good and bad in my assessment. First, you have to take a moment to really look at them - that is bad in today’s world. The red and orange are worse toxicity outcomes and simply those outcomes are only found in the IMRT arm. (Granted, you could set the color key different for this non-verified metric and, while the trend would persist, the color differences might be less dramatic).
In figure (A) below, you see 4 data groups: Surgery IMRT, No surgery IMRT and then Surgery Proton and No surgery proton groups. The biggest difference is in the surgically treated arms - compare the top grouping (Surgical IMRT) to grouping 3 (Surgical Proton). (All the red colors indicate high toxicity outcomes which are concentrated in the IMRT surgical arm).
In figure (B) below, we see labels like PNA (pneumonia) and AFIB (atrial fibrillation). The key to the abbreviations is the table 1 I included above from the TTB reference article. It has a second division: the left half (vertically) are chemotherapy / radiation toxicities and the right half (RED labels starting with “AL”) are post-operative complications - so actually 8 data sets of relative toxicities.
This 2nd figure again shows greater toxicity in the IMRT arm with the worst toxicities concentrated in those having surgery.
Note: If you are just reading the paper - this graphic was actually merged into one visual. It was so much information, I had to break it up into components to even attempt to explain it. Secondly, the abbreviations are only in the figure text and the relative weightings are not in the final publication - you have to cross-reference the original total toxicity reference document for that information as we presented above.
These are pretty clear graphics if this has been your life’s research for the better part of a decade. But as an outsider, they are terribly complex. I think that complexity ultimately renders them far less impressive rather than some simple metric that you can read and appreciate in one sentence - like “Gr3 toxicities were greater by xxx amount.”
Here are two items from the supplemental data PDF that, to me, are simpler. The first shows that toxicity is worse with IMRT. Basically outcomes farther left have less toxicity and farther right have more - and IMRT is clearly to the right of proton therapy IMRT outcomes.
It is quite clear these treatments do not result in the same outcomes, albeit the figure is derived from math on top of a rather complex baseline metric.

And finally, the graph below shows Grade 4 lymphopenia comparisons illustrating the type of Grade 4 toxicity differences at various time points. Lymphopenia - problems related to low blood counts are significant. Grade 4 toxicity in our literature is more broadly correlated with overall survival. (ref 3,4,5) This is relatively well established and likely represents one of the major pathways in which protons have potential to improve outcomes.

In summary, I view this as very strong data. It is most convincing / most different in those undergoing surgery, which is the group that will have the best long-term outcomes and therefore have the most potential benefit.
I don’t love the presentation of the trial due to complexity, but protons (even with passive scatter used in 80%) outperformed IMRT at a world class leading institution for concurrent esophageal cancer treatment.
Why so little uptake? Why not standard of care?
Here is the argument against the data above:
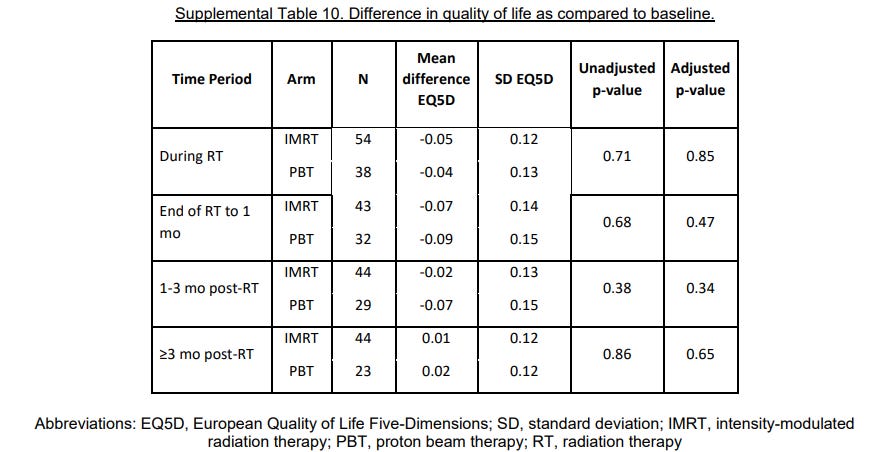
Patient Quality of life data - I’ll summarize, nothing different.
And progression free survival and overall survival - no difference.
(but consistent with design - remember same dose of 5040).
And therein lies one of two major problems:
To appreciate the upside, you need time / energy / effort. To understand the downside, just list off the patient quality of life and progression free / overall survival data.
Paragraphs for the upside explanation and literally “no difference” for the downside explanation. And today’s world runs on headlines.
What is issue two? It’s a proton trial.
When studies align with where “we” think medicine should go, we accept sometimes little to no data. When it doesn’t align with our interest or it is hard to accomplish, the bar is set far higher.
Take my home state of Arkansas where I practiced for 20 years. Today, it has zero proton machines - do you really believe that all thoracic surgeons in tumor board who are most likely employees of a hospital will refer patients out of state based on one trial? No. It doesn’t align with the interest of the medical community or their hospital, and even if they considered it, that process is time consuming and made to be difficult.
In European countries, I think we are beginning to see these types of referral patterns develop around proton therapy - prioritizing across a country which patients benefit most and optimizing the use of protons in those patient subsets. But in the US? Those systems do not exist and they strongly conflict with our hospital structure where referrals - beyond the walls of the institution are dis-incentivized on many levels.
What happened in the patient quality of life data?
Physician toxicity metrics and patient toxicity metrics measure different things - they can both be useful. In prostate cancer for example, high grade toxicity is so limited and infrequent that the only way to measure slight toxicity changes are via patient survey data regarding quality of life. Waking up once vs. three times at night is easier to pick up in a patient survey. Same thing for mild bowel urgency that isn’t enough for most to take Imodium - these are subtle changes - real, but subtle. You are searching for differences in a sea of Grade 0 to mild Grade 2 toxicities.
Compare that to here - here we have major ICU causing events happening at 7.6 times the rate in IMRT arm in those having curative surgery. But on surveys, both populations got really sick, both had plenty of toxicity compared to normal life with major life changes, and both treatment arms are now happy to be around - literally. Perspectives matter.
Both tools can be useful to evaluate outcomes. But my stance is to not discard a difference in major post-operative complications due to a patient outcome quality of life survey where patients must prioritize fighting for survival. (unfortunately that is the seriousness of this disease)
Would I see this type of impact on side effects?
Honestly, I think this is the floor for the difference between IMRT and proton therapy outcomes. This was at MD Anderson - a great multi-disciplinary team, experienced super high volume surgeons and radiation oncologists with experienced hospital care teams - the number one rated cancer hospital year after year.
Surgery after radiation is risky - experience should minimize that risk. If IMRT made it more difficult for these surgeons, it probably has a larger difference for your surgical and post-operative care team. That would be my generalized guess.
My summary:
The deeper I look, the more this trial does in fact demonstrate a very significant win for proton therapy.
Restating the results: In patients undergoing surgery, the mean post-operative complication score was 19.1 (CI 7.3-32.3) versus 2.5 (CI 0.3-5.2). Stated differently, the risks of anastomotic leaks, ARDS (shutting down of lungs), pulmonary embolism, reintubation, stroke, and post-operative pneumonia and atrial fibrillation were 7.6 times more greater if treated with IMRT instead of PBT.
(Read that paragraph again - it is a large scale difference. It does include a weighting metric you must agree with, but even if you don’t think the weighting is perfect, complications are still worlds apart. )
To me, these are clearly different toxicity outcomes - as strong as any IMRT vs 3D conformal data.
Unfortunately some of outcome differences in this trial, from my perspective, got buried in the presentation and publication. I was in the room during the data presentation and it didn’t feel like “a big win”. But looking back and looking much deeper, I don’t think that is the case, but in today’s world 98% will never look again. First impressions matter.
The problem was / is. On first glance QoL, PFS, OS - all the same. So very easy statements of “no difference” easily wash away a benefit seen in a new rather complex toxicity metric. Total Toxicity Burden is a metric that takes any well educated reader probably 30 minutes (minimum) time to have any chance to really interpret for themselves across multiple references. No trial is perfect and in hindsight, the choice of total toxicity burden as a primary metric appears to weigh heavily on the assessment of outcome in this trial.
But as a patient, if diagnosed, I’d at least head to the National Association for Proton Therapy and consider my personal options for where I might discuss proton therapy - especially if I was young enough / strong enough to have surgery after radiation and chemotherapy. If you wish to participate in the current national trial that essentially is repeating this trial with pencil beam approaches and a simpler grade 3 toxicity outcome metric look here: NRG-G1006, NCT03801876.
Outside of you taking initiative and asking, I think it is highly unlikely this option will even be mentioned if you are not at a center with access to proton therapy. And to me as we reviewed today, the best data we have suggests that proton therapy is the less toxic treatment approach.
Kudos to Steven Lin and the team at MD Anderson for getting this trial completed!
REFERENCES:
Esophageal Cancer Randomized Trial:
https://ascopubs.org/doi/10.1200/JCO.19.02503Bayesian / Total Toxicity Burden Design Publication:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4809549/Severe Radiation-Induced Lymphopenia Affects the Outcomes of Esophageal Cancer: A Comprehensive Systematic Review and Meta-Analysis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9221375/The Influence of Severe Radiation-Induced Lymphopenia on Overall Survival in Solid Tumors: A Systematic Review and Meta-Analysis
https://pubmed.ncbi.nlm.nih.gov/34329738/Radiotherapy-Related Lymphopenia Affects Overall Survival in Patients With Lung Cancer
https://www.jto.org/article/S1556-0864(20)30478-0/fulltext