Protons 101: ORIGINAL PUBLICATION, Dysphagia-Optimized Unilateral Proton Radiation Therapy: A Comparative Study Evaluating Constrictor Muscle Dosimetry
Study evaluating dose to the pharyngeal constrictors in unilateral head and neck cancer radiation treatment. Authors: Mark R Storey MD, Suresh Rana MS
Quick Note: This is a 100% technical medical literature post.
Purpose:
This study reports dose delivered to the superior middle pharyngeal constrictors muscles (SMPCM) and the inferior posterior constrictor muscles (IPCM) utilizing proton therapy compared to dysphagia-optimized IMRT (Do-IMRT) in unilateral head and neck treatment.
Patients and Methods:
8 consecutive patients, previously treated at the Oklahoma Proton Center with unilateral radiation for head and neck cancer, were evaluated. Using original target volumes, we generated 4 treatment plans for comparison: 1) standard IMRT (S-IMRT) (no pharyngeal constrictor constraints), 2) Do-IMRT (created per DARS trial constraints), 3) uniform scanning proton therapy (USPT), and 4) pencil beam scanning (PBS) proton therapy. Both USPT and PBS utilized a dysphagia optimized planning approach.
Results:
The study included 4 base of tongue, 2 tonsil, 1 oral tongue (post-operative) and 1 parotid (post-operative) cases. Do-IMRT significantly reduced IPCM and SMPCM mean dose compared to S-IMRT (p<0.001, p=0.002, respectively). Both USPT and PBS reduced mean dose compared Do-IMRT to the IPCM (p<0.001 for both comparisons). USPT reduced mean dose to the SMPCM compared to S-IMRT (p=0.026) but did not reduce mean dose when compared to Do-IMRT (p=0.139). PBS reduced mean dose to the SMPCM compared to Do-IMRT (p=0.006). PBS reduced mean dose to the SMPCM compared to USPT (p<0.001) and trended lower for IPCM mean dose although not meeting significance (p=0.06).
Conclusion:
Do-IMRT appears to significantly narrow the margin of dosimetric improvement between proton therapy and S-IMRT. PBS proton therapy continues to show significant improvements in the ability to spare pharyngeal constrictors and markedly reduces normal OAR dose. USPT failed to reduce dose to the SMPCM compared to Do-IMRT but did maintain dosimetric advantages for the IPCM, larynx, oral cavity, and lips. Ongoing trials comparing protons and photons should move towards Do-IMRT to ensure an accurate clinical comparison to the new standard of care for IMRT.
Keywords: Proton therapy, radiation, Unilateral, Dysphagia-Optimized
Introduction
Treatment related toxicity is a primary consideration for the treatment of head and neck cancer. The role of proton therapy is increasing as an avenue to reduce toxicity [1-3]. There is a constant push to reduce toxicity either with improved surgical techniques or through improvements in radiation delivery [4,5]. Standard of care by site is often determined not only by local control or survival data, but quality of life and toxicity implications of the treatment approach [6].
Recently, data from the dysphagia/aspiration at risk structures (DARS) trial was presented [7-9]. It showed improved patient reported swallowing function when dose to the superior middle pharyngeal constrictor muscles (SMPCM) and the inferior pharyngeal constrictor muscle (IPCM) was reduced using strict dose constraints in the development of IMRT plans. The trial compared standard IMRT (S-IMRT) to dysphagia-optimized IMRT (Do-IMRT). In the standard arm, the pharyngeal constrictors were not contoured and in contrast, in the Do-IMRT the SMPCM and IPCM were contoured and constraints were set to attempt to limit mean dose to <50 Gy and <20 Gy respectively. Clinical outcome data from the trial showed this Do-IMRT was able to reduce dose to the SMPCM from 57.2 Gy to 49.7 Gy and for the IPCM from 49.8 Gy to 28.4 Gy for the S-IMRT and Do-IMRT arms respectively. These dose difference resulted in improved clinical outcomes and no additional local failure risk. We believe this dose reduction and resulting improvement in the clinical outcomes represents the first dosimetry metric to be proven in a randomized prospective clinical trial.
At the same time in our field, proton therapy is increasingly being studied for the treatment of head and neck cancer. Its use in the treatment of head and neck cancers has increased in recent years as the technology has continued to progress from scatter approaches with aperture and compensator treatments to pencil beam approaches [10]. There is increasing evidence that proton therapy has the potential to reduce toxicity compared to IMRT for the treatment of pharyngeal cancers with multiple very important clinical trials in progress [1]. This study seeks to determine if proton therapy maintains dosimetric advantages when compared to this newly established Do-IMRT to allow for the further reduction of dose to the pharyngeal constrictors.
Patients and Methods
8 consecutive patients that had been previously treated at the Oklahoma Proton Center were utilized in this institutional review board approved dosimetry study. Patient’s CT datasets were transferred and anonymized into a clinical research server. To create a consistent comparison, original treatment plans created within our clinical Xio environment were not utilized for this study. Dose level recommendations were maintained according to the original treating prescriptions to attempt to decrease potential biases. Four new representative treatment plans were created with RayStation planning software for each dataset. Comparisons between datasets are performed using a two-sided, paired T-Test. Of note for our unilateral approach which utilizes USPT, we utilize a head turned / open neck approach. The goal is to create a flat even surface while attempting to limit depth differences so that the inverse-square effects are minimalized. In simple terms, this is more akin to a setup using electrons allowing uniform dose and good coverage of the cervical lymph node at risk.
S-IMRT and Do-IMRT plans were created according to the DARS trial attempting to mirror the approach within the original study protocol. Note in the Do-IMRT arm, low dose coverage is compromised if needed to meet SMPCM and IPCM constraints. Intermediate and high-risk dose regions are not compromised. In general, planning objectives were prioritized as follows within the two IMRT arms:
1)S-IMRT: critical organ constraints (spinal cord and brainstem): PTV coverage, parotid gland constraints, other head and neck structures including oral cavity, larynx, opposite submandibular gland as feasible.
2)Do-IMRT (followed by USPT and PBS as well): critical organ constraints (spinal cord and brainstem): Intermediate and high dose PTV coverage, constrictor constraints, low dose PTV coverage, parotid gland constraints and other head and neck structures as feasible.
Proton therapy plans were generated using both a USPT and PBS approach. Uniform scanning beam model is based on the IBA proton therapy system with a universal nozzle [11]. PBS beam model is based on IBA ProteusPLUS proton system with PBS dedicated nozzle [12, 13]. The uniform scanning proton therapy plan was created with PTVs identical to IMRT plans. Pencil beam scanning proton therapy plans were calculated using multi-field optimization (MFO) technique in conjunction with the robust optimization (3 mm setup uncertainty and 3.5% range uncertainty). Robust objective was applied to the CTVs only. For PBS plans, Monte Carlo algorithm was used for both plan optimization (10,000 ions/spot) and final dose calculations (0.5% statistical uncertainty), whereas uniform scanning plans were computed using pencil beam algorithm. In addition, PBS plans were generated using a robust optimization technique. Plan robustness evaluation was performed for the PBS plans. Specifically, PBS plans were evaluated for the isocenter shift of X = ±3 mm, Y = ±3 mm, and Z = ±3 mm. Range uncertainty was investigated for ±3.5%. If the CTV has D95% ≥98%, the plan was considered as robust. Prescribed radiation doses for the two proton approaches used a relative biological effectiveness (RBE) value of 1.1.
The following clinical goals were utilized to create a standardized review of the 4 plans:
Spinal cord OAR < 5000 cGy absolute maximum dose
Maximum plan hot spot: 110% of prescribed dose to <1cc
Coverage of intermediate and high dose target volumes at 98% coverage at 98% of prescription
Coverage of the low risk target volume at 98% coverage and 98% of prescription was performed assuming that the IPCM and SMPCM constraints were met.
IPCM mean dose < 2000 cGy*
SMPCM mean dose < 5000 cGy*
*S-IMRT: No IPCM/SMPCM goal, instead larynx reduced to 3500-4000 cGy consistent with Danish Head and Neck Cancer group Radiotherapy Guidelines 2019 [14].
Fundamentally uniform scanning plans differ from both IMRT and PBS techniques. IMRT and PBS can utilize various dose rates simultaneously throughout a single course of treatment in today’s clinical environment utilizing a simultaneous integrated boost approach (SIB). S–IMRT and DO–IMRT plans were generated using an SIB approach to deliver 6996 cGy in 33 fractions to areas of high risk. Intermediate risk volumes were treated to 6000 cGy. Low risk volumes were treated to 5400 cGy. This same approach SIB approach was utilized for pencil beam proton therapy planning creating single plans. In contrast, uniform scanning proton therapy plans are more consistent with older 3-D treatment approaches where the entire volume receives the same dose per fraction using a reduction in volume to create the boost fields. Therefore, all USPT plans were created using a conventional sequential technique delivering 7000 cGy(RBE), 6000 cGy(RBE), and 5000 cGy(RBE) respectively to the high, intermediate, and low risk regions with all treatments delivered at 200 cGy(RBE) per fraction. We felt this was the most pragmatic approach to replicate plans that would be implemented within the clinic. Three cases were treated to a total dose less than 7000 cGy (6400 cGy for 2 cases and 6600 cGy for 1). In these cases, the highest dose was planned at 200 cGy per fraction for 32 and 33 fractions, respectively.
Results
Patient population is shown below in Table 1. As shown, patients consisted largely of HPV+ patients with primary sites being in the tonsil or earlier stage and more lateralized base of tongue lesions. 3 cases were post-operative and therefore were treated to doses in the mid 6000 cGy level.
The results presented in our study are from the nominal plans. Plans for all 8 patients using all techniques were successfully created and able to meet coverage and spinal cord / brainstem constraints. A representative case showing the 4 different approaches is shown in Figure 1.
Figure 1: Representative Single Slice Examples of the 4 plan approaches generated for each case: S-IMRT, Do-IMRT, USPT, PBS
a) S-IMRT, b) Do-IMRT, c) USPT: Uniform scanning proton therapy, d) PBS; Pencil Beam scanning proton therapy.
For a single case (Table 2, T2N1 patient(*)), Do-IMRT and USPT could not meet the IPCM goal of <2000 cGy at 3146 cGy and 2304 cGy respectively even after compromising coverage of the low dose PTV. For the same patient Do-IMRT resulted in a dose of 5413 cGy to the SMPCM also failing to meet optimal treatment criteria. For our PBS plans, the worst-case-scenario results from the plan robustness showed that 7 out of 8 patients met the robustness criteria with a single case failing to maintain CTV coverage D95% ≥98% for all scenarios.
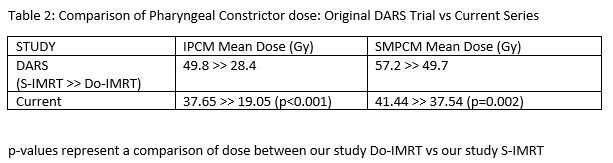
The initial analysis attempted to verify that the DARS trial data was replicated on some reasonable level within our small sample. In our study, Do-IMRT reduced mean dose to both the IPCM and SMPCM in a fashion that appears comparable to the original trial design achieving a statistically significant reduction in dose to both the IPCM and SMPCM. Results comparing our study dosimetry to the DARS trial is shown in Table 2.
Dosimetry results for the 4 unilateral head and neck approaches are shown in Table 3.
Integral dose was significantly reduced in the proton therapy plans compared to the two photon plans with the proton plans delivering an integral total dose of approximately 46% of the integral dose delivered with photons (p<0.001 photon vs proton) for this patient population. Ipsilateral parotid dose was evaluated in 7 cases (case 6, ipsilateral parotid tumor was excluded). Mean dose was highest in the USPT group (4585cGy(RBE)) but based on less consistency and a larger variance, no comparison reached significance (nearest, p=0.081 compared to S-IMRT). Do-IMRT did have a statistically higher ipsilateral parotid dose compared to S-IMRT (4102 cGy vs 3912 cGy, p=0.0214). PBS produced the lowest ipsilateral parotid dose at 3509 cGy(RBE) and neared significance compared to both USPT (p=0.0938) and Do-IMRT (p=0.0659).
Discussion
The DARS trial was a landmark trial for proving value in a dosimetry metric. From our work in this study, it is very apparent that the approach as described in the DARS study creates a strong prioritization of the pharyngeal constrictors within an IMRT framework. This, in turn, creates a rather reliable and reproducible planning result. Based on the specific protocol that emphasizes a dramatic reduction in dose to the pharyngeal constrictors, there is very little room to adjust other organs at risk while meeting tumor coverage and spinal cord constraints. In contrast S–IMRT allows for significantly greater flexibility in shifting priorities which appears to allow for a significant level of variation depending upon the exact optimization pattern and the exact level with which each constraint is pushed during the optimization process.
The second notable feature of the study is that the comparisons between the dysphagia optimized IMRT and proton therapy were significantly closer than comparisons with S–IMRT. Even with the small sample size, you see USPT losing the ability to significantly reduce dose to the SMPCM when compared to Do-IMRT. In our experience for unilateral head and neck radiation, strongly prioritizing the optimization of the pharyngeal constrictors via the DARs protocol, many OAR structures (such as the larynx and opposite parotid) are optimized without further constraints or objectives by strongly optimizing the pharyngeal constrictors which inherently moves dose away from these organs at risk. High level pharyngeal optimization potentially has some slight negatives in allowing less flexibility with dose to the lips and/or oral cavity, but it has clear clinical benefit based on published data [8]. Based on our work, this approach has significant benefits in generating a far more consistent and reproducible IMRT plan. The original authors and developers of that work deserve great credit for their contribution and documentation of their approach leading up to, during, and since the completion of the trial. We believe that it was able to be validated, in part, due to this reproducibility which then adds significant value as a clinical recommendation.
Both uniform scanning and pencil beam scanning proton therapy plans were able to create significant advantages over Do–IMRT planning. There was a significant reduction in dose to the oral cavity, larynx, and lips with either proton therapy approach significantly reducing dose to each of these normal structures that are related to acute toxicity. It should be noted that while USPT was not statistically worse concerning ipsilateral parotid dose, USPT did yield the highest mean value for the ipsilateral parotid. Clinically it also produces a higher skin dose than IMRT approaches. The higher skin dose combined with this potential parotid higher dose represent important reasons that scatter based proton treatments require further clinical validation versus high quality IMRT. It should be noted that, in our study, parotid dose was higher using Do-IMRT compared to S-IMRT, therefore it is possible that lower parotid dose is far less important than dose to central structures of the head and neck region.
There was an expected significant decrease in integral dose with proton therapy plans over the IMRT plans delivering less than half of the integral radiotherapy dose in these unilateral treatment plans. Unlike many sites where acute toxicity is much more limited, integral dose is far more linked with acute side effects and acute toxicity in the head neck region [15]. While long-term reduction in second malignancies may be a potential real benefit for protons [16], we believe the major clinical differences for integral dose in the treatment of head and neck cancer is a reduction in acute toxicity and improvements of QoL within the initial 2-5 years of treatment. Certainly, dose to the oral cavity, lips, and pharynx are critical to tolerance of treatment and these dramatic overall dose reductions certainly appear to be consistent with a treatment approach that will be far better tolerated and generate faster recovery.
The utility of unilateral focused radiation therapy head and neck cancer is a revolutionary treatment concept shift in head and neck radiation therapy. Historically, we have moved from the days of 3 field comprehensive head and neck radiation to 3-dimensional conformal radiation to IMRT, but continuing the dogma of comprehensive radiation to nodal regions at risk based upon historic surgical data. Now, even with the particle therapy approaches, we are often still practicing the same paradigm. More data are available now for comparable non-inferior outcomes with unilateral approaches. Recent data from Australia in 2018 by Tiong et al [17] revealed that in human papilloma virus mediated squamous cell carcinomas of unknown origin, there were no isolated contralateral lymph nodal failures in patients treated to the ipsilateral neck alone, while there was 1 contralateral failure with an associated distant failure in the 49 patients studied. From the Washington University, Chin et al in 2017 [18] published their collective experience (prospective and retrospective) on 154 patients treated with oropharyngeal cancer with bilateral versus unilateral neck coverage. Even with lymph nodal positive disease, the omission of contralateral neck nodes did not affect the local control or overall survival at a median follow up of over 5 years. Finally, a review of the literature by the group from the Netherlands Al-Mamgani et al in 2017 [19] revealed 11 published studies with a combined total 1116 patients treated with ipsilateral neck radiation. The contralateral neck failure rate was only 2.4% overall, with the highest risk of course being more midline lesions with a 12.1% contralateral failure. Thus, many patients in the past and even currently are being over treated when bilateral neck nodal coverage is employed.
This study has weaknesses primarily being no related clinical outcomes and a limited study size that includes a variety of tumor sites. Certainly, the small numbers of patients limit the confidence and power of our statistical analysis. That said, we do believe that this analysis can serve a starting point in beginning to establish comparisons for proton therapy when compared to the new standard Do-IMRT. While the statistical analysis should be viewed within the context of study sample size, the statistical analysis did support and seem very consistent with our teams review of the differences that we appreciated within the various plan approaches.
As with any dosimetry trial, there is always a question of plan optimization techniques and whether the results would be reproducible in the hands of other radiation oncology teams. We will discuss three primary aspects of this study favor its reproducibility. The first is experience. For both IMRT and USPT plans, the team has decades of experience in generating plans for the treatment of head and neck cancer. In contrast, the PBS experience represents a small fraction of the IMRT and USPT experience and we believe that, if anything, this would bias the study against PBS as a superior approach. Secondly, the study allowed for far greater time to be spent on optimization of the plan that is often available in the clinic. While the small sample size is detrimental in many ways, the small number of cases allowed for repeated iterations of the plans against the other plans as we searched for the optimal approach for each technique. Finally, this study produced multiple plans per patient using very different approach. During treatment planning, we were able to utilize information from all approaches to help in our optimization. We believe that this ability to plan against various approaches helped achieve a higher level of overall plan optimization for all approaches.
The DARS trial was more specifically for bilateral cases and clearly this study attempts to transition and evaluate that approach within a unilateral subset of patients. Our center historically is a uniform scanning center and therefore has treated a much more limited number of cases in the head and neck region. Based on that history, we have largely centered on unilateral cases. While there is likely less relative benefit for the treatment of a unilateral case than a bilateral case [20], unilateral treatment is still quite toxic with significant acute toxicity. Based on this work, we do believe that the dysphagia-optimized approach parameters described can be effectively utilized within a unilateral approach with no further changes aside from a general expectation to have lower mean doses for both the SMPCM and IPCM.
In summary, the recent DARS trial showing that Do–IMRT causes significantly less toxicity than S–IMRT helps to establish a new standard for IMRT in the treatment of head and neck cancers. Based on this study, Do-IMRT likewise appears to decrease the dosimetry differences between proton therapy and IMRT. However, there are still significant decreases in the dosimetry parameters to the pharyngeal constrictors from proton therapy (PBS more so than USPT). This is encouraging as we transition our center to PBS and more current centers utilize PBS. We encourage ongoing and future head and neck trials for both photon and proton modalities to integrate pharyngeal constrictors sparing consistent with the dysphagia optimized approach presented in the DARS trial. To establish the possible benefit of proton therapy over the highest standard of IMRT, pharyngeal constrictor parameters need to be followed as a critical OAR moving forward.
Reference List:
1. Li X, Lee A, Cohen MA et al. Past, present and future of proton therapy for head and neck cancer. Oral Oncology Volume 110, Nov 2020; 110: 104879.
2. Kandula S, Zhu X, Garden AS, et al. Spot-scanning beam proton therapy vs intensity-modulated radiation therapy for ipsilateral head and neck malignancies: a treatment planning comparison. Med Dosim 2013;38(4):390–4.
3. Aljabab S, Liu A, Wong T, Liao JJ, et al. Proton Therapy for Locally Advanced Oropharyngeal Cancer: Initial Clinical Experience at the University of Washington. Int J Part Ther. 2019;6(3):1-12.
4. Nichols AC, Theurer J, Prisman E, et al. Radiotherapy versus transoral robotic surgery and neck dissection for oropharyngeal squamous cell carcinoma (ORATOR): an open-label, phase 2, randomized trial. Lancet Oncol. 2019;20:1349–59.
5. Gupta T, Agarwal J, Jain S, et al. A. Three-dimensional conformal radiotherapy (3D-CRT) versus intensity modulated radiation therapy (IMRT) in squamous cell carcinoma of the head and neck: a randomized controlled trial. Radiother Oncol. 2012 Sep;104(3):343-8.
6. Grover S, Swisher-McClure S, Mitra N, et al. Total Laryngectomy Versus Larynx Preservation for T4a Larynx Cancer: Patterns of Care and Survival Outcomes. Int J Radiat Oncol Biol Phys. 2015 Jul 1;92(3):594-601.
7. Nutting C, Rooney K, Foran B, et al on behalf of the DARS Investigators. Results of a randomized phase III study of dysphagia-optimized intensity modulated radiotherapy (Do-IMRT) versus standard IMRT (S-IMRT) in head and neck cancer. J Clin Oncol May 20, 2020; 38(15_suppl) 6508-6508.
8. Petkar I, Rooney K, Roe JWG, et al. DARS: a phase III randomised multicentre study of dysphagia- optimised intensity- modulated radiotherapy (Do-IMRT) versus standard intensity- modulated radiotherapy (S-IMRT) in head and neck cancer. BMC Cancer. 2016;16:770.
9. Feng FY, Kim HM, Lyden TH, et al. A. Intensity-modulated chemoradiotherapy aiming to reduce dysphagia in patients with oropharyngeal cancer: clinical and functional results. J Clin Oncol 2010; 28(16): 2732-2738.
10. Mohan R, Grosshans D. Proton therapy - Present and future. Adv Drug Deliv Rev 2017;109:26–44.
11. Rana S, Eckert C, Singh H, Zheng Y, Chacko M, Storey M, Chang J. Determination of machine-specific tolerances using statistical process control analysis of long-term uniform scanning proton machine QA results. J Appl Clin Med Phys. 2020 Sep;21(9):163-170. doi: 10.1002/acm2.12990. Epub 2020 Aug 1. PMID: 32741135; PMCID: PMC7497929.
12. Rana S, Bennouna J. Investigating beam matching for multi-room pencil beam scanning proton therapy. Phys Eng Sci Med. 2020 Dec;43(4):1241-1251. doi: 10.1007/s13246-020-00927-7. Epub 2020 Oct 6. PMID: 33025387.
13. Rana S, Bennouna J, Gutierrez AN, Rosenfeld AB. Impact of magnetic field regulation in conjunction with the volumetric repainting technique on the spot positions and beam range in pencil beam scanning proton therapy. J Appl Clin Med Phys. 2020 Oct 15;21(11):124–31. doi: 10.1002/acm2.13045. Epub ahead of print. PMID: 33058380; PMCID: PMC7700936.
14. Radiotherapy Guidelines 2019 Danish Head and Neck Cancer group. URL: https://www.dahanca.dk/assets/files/GUID_DAHANCA%20Radiotherapy%20Guidelines%202019.pdf
15. Frank SJ, Blanchard P, Lee JJ, et al. Comparing intensity-modulated proton therapy with intensity-modulated photon therapy for oropharyngeal cancer: the journey from clinical trial concept to activation. Semin Radiat Oncol. 2018; 28 (2): 108– 13.
16. Jain V, Irmen P, O'Reilly S, et al. Predicted Secondary Malignancies following Proton versus Photon Radiation for Oropharyngeal Cancers. Int J Part Ther. 2020;6(4):1-10.
17. Tiong A, Rischin D, Young RJ, et al. Unilateral radiotherapy treatment for p16/human papillomavirus-positive squamous cell carcinoma of the unknown primary in head and neck. Laryngoscope 2018; 128: 2076-83.
18. Chin RI, Rao YJ, Hwang MY, et al. Comparison of Unilateral Versus Bilateral Intensity-Modulated Radiotherapy for Surgically Treated Squamous Cell Carcinoma of the Palatine Tonsil. Cancer 2017; 123: 4594-607.
19. Al-Mamgani A, Verheij M, van den Brekel MWM. Elective unilateral nodal Irradiation in head and neck squamous cell carcinoma: A paradigm shift. Eur J Cancer 2017 Sep; 82: 1-5.
20. Tambas M, J H M Steenbakkers R, van der Laan HP, et al. First experience with model-based selection of head and neck cancer patients for proton therapy [published online ahead of print, 2020 Aug 5]. Radiother Oncol. 2020;S0167-8140(20): 30715-5.
Note: Original publication and research work self publication - so not a “peer reviewed publication”.
Why Substack? I wrote this back in 2020 - and I have now submitted the paper x2 with really no final answer either time - minor edits only but never got it pushed over the finish line x2. It isn’t a landmark trial and patient numbers are small - I get that. But at some point, I just need to move along - better here than on my hard drive. To me, it illustrates what you see in a planning environment with current approaches with proton therapy showing a dosimetric advantage. The randomized OPC proton vs. photon trial will give a definitive answer - it has completed accrual and we’re waiting on data analysis.